 A team of Portuguese researchers has uncovered an important cellular cross-talk promoting ovarian cancer growth.
A team of Portuguese researchers has uncovered an important cellular cross-talk promoting ovarian cancer growth.
According to the American Cancer Society, there are approximately 21,980 new cases of ovarian cancer every year, making it the fifth leading cause of cancer-related death among women, and the deadliest of gynecologic cancers.
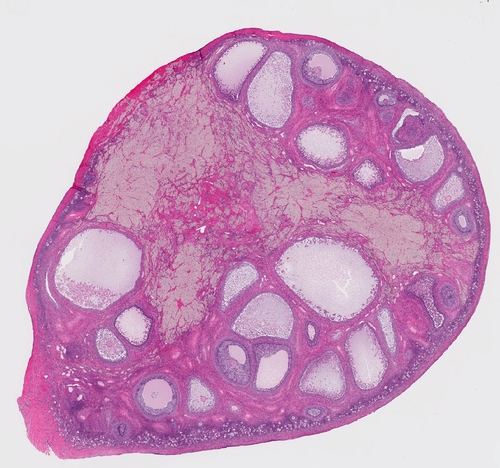
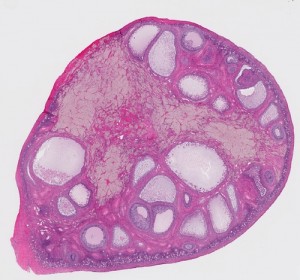
The study, entitled “Murine CD27(−) Vγ6(+) γδ T cells producing IL-17A promote ovarian cancer growth via mobilization of protumor small peritoneal macrophages” and published in the renowned Proceedings of the Natural Academy of Sciences of the USA (PNAS) journal, assessed a mouse model of peritoneal/ovarian cancer, demonstrating that a specific type of T lymphocytes, γδ (gamma-delta) T cells, accumulate in the peritoneal cavity upon tumor challenge and are responsible for promoting tumor cell growth.
It is known that cancer-associated inflammation is responsible for the mobilization of several immune cells that can either inhibit or promote tumor growth. γδ T cells have the capacity to infiltrate the tumor microenvironment and are commonly thought to release anti-tumor cytokines, this way generating an immune response against cancer cells.
“Contrary to the well-established anti-tumor function of γδ T cells, which we and others have previously documented in melanoma and leukemia, this study describes their pro-tumor function in a murine model of ovarian cancer” lead author of the study Bruno Silva-Santos, PhD, Instituto de Medicina Molecular (IMM), Lisbon, told Immuno-Oncology News.
Upon functional characterization of tumor-associated γδ T cells, the researchers observed that these cells were producing interleukin-17A (IL-17), a cytokine responsible for recruiting monocytes and neutrophils to sites of inflammation and commonly associated with poor prognosis in cancer settings.
Accordingly, they found that IL-17 was mobilizing small peritoneal macrophages (SPM) to the tumor site, which were directly responsible for promoting ovarian cancer cell proliferation. Furthermore, mice lacking either γδ T cells or IL-17 exhibited reduced tumor growth when compared with normal control animals.
“The IL-17 produced by γδ T cells mobilizes SPM’s endowed with direct pro-angiogenic and pro-tumor (proliferative) functions. Thus, we identified a pathogenic γδ T cell/ IL-17/ SPM axis that can be a new therapeutic target in immuno-oncology. Work by others has been validating the pathogenic role of IL-17-producing γδ T cells in patients and in other cancer types. For example, these cells are a bad prognosis marker for colorectal cancer patients. Future research should therefore explore the neutralization of IL-17 (for example, using the antibodies currently being used in psoriasis) as a novel approach in cancer immunotherapy,” added Dr. Silva-Santos in his exclusive interview with Immuno-Oncology News.
The study, a collaboration between IMM and the Queen Mary University of London researchers, included first author Margarida Rei, Natacha Gonçalves-Sousa, Telma Lança, Richard G. Thompson, Sofia Mensurado, Frances R. Balkwill, Hagen Kulbe, Daniel J. Pennington and Bruno Silva-Santos.