Researchers have uncovered the mechanism behind a previously unexplained phenomenon, where local radiation of a tumor causes tumors in other body parts to shrink.
Findings showed that radiation caused tumor-associated immune cells, called neutrophils, to die. The dead cells were replaced by new neutrophils, which attacked both the irradiated tumor and those in other parts of the body. Importantly, researchers discovered the response could be boosted with a natural immune factor.
The study, “Key role for neutrophils in radiation-induced antitumor immune responses: Potentiation with G-CSF,” was published in the journal Proceedings of the National Academy of Sciences (PNAS).
Scientists have long known that radiating a primary tumor sometimes can make other tumors in the body shrink. Physicians refer to this as the “abscopal effect.” But so far, no one has been able to explain how it happens.
“The abscopal effect is only seen sporadically, but when it does happen, the effect induces a long-lasting, anti-tumor response in patients,” Raquibul Hannan, MD, senior author of the study, said in a news release. Hannah is an assistant professor of Radiation Oncology and a member of the Harold C. Simmons Comprehensive Cancer Center at University of Texas Southwestern Medical Center in Dallas.
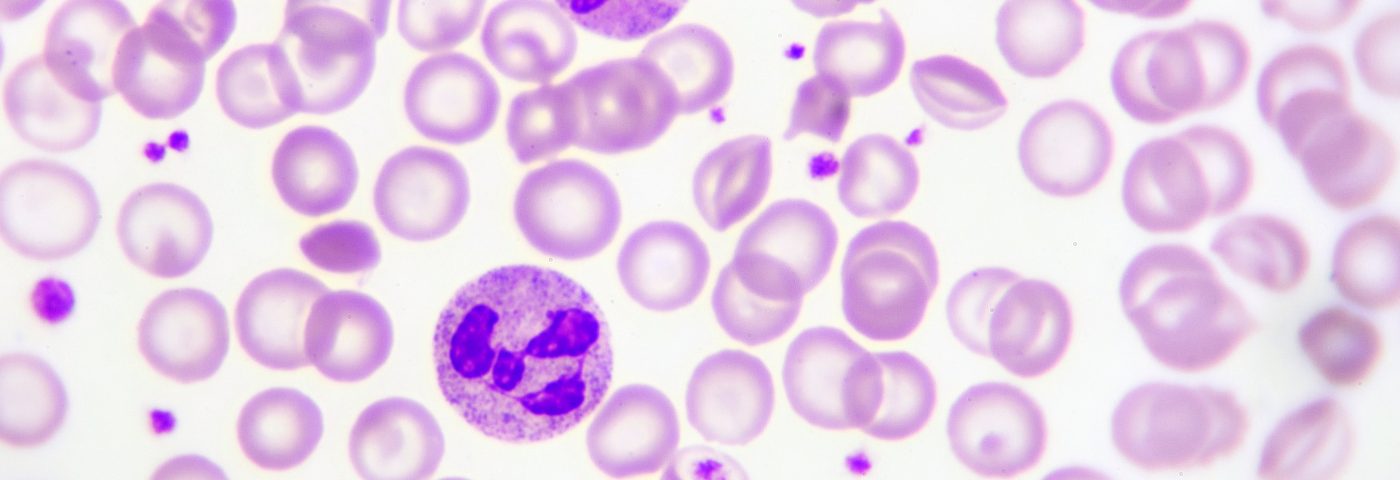
The research team used mice as models to understand the phenomenon, and discovered that neutrophils are key players in this response. Immune cells, such as neutrophils, are set up to fight cancer cells. But many cancers use strategies that, instead, make immune cells run the tumor’s errands, helping it to grow.
When the primary tumor in the mice was irradiated, researchers noted the tumor-associated neutrophils died. This recruited new neutrophils to the site, and since they had not been subdued by the tumor, they attacked both the primary tumor, and spread through the body to attack also other tumors.
The study also showed that the newly activated neutrophils, in turn, activated immune T-cells to fight the cancer.
“To our knowledge, this is the first study to identify radiation-induced neutrophils and to demonstrate their anti-tumor activity via both innate and adaptive immune responses,” said Tsuguhide Takeshita, MD, instructor in Radiation Oncology and lead author of the study.
In an experiment that further increased the usefulness of the findings, the research team was able to show that giving mice G-CSF (granulocyte colony-stimulating factor) before the radiation, triggered the capacity of the activated neutrophils to kill cancer cells.
G-CSF is an immune factor present naturally in the body and involved in the production of neutrophils and other immune cells. The factor already is used in the clinic to treat conditions where patients lack such cells.
“These results provide support for evaluating the combined use of radiation therapy and G-CSF in pre-clinical and clinical settings,” said Hannan, adding that the long-term goal of the team is to do away with the sporadic nature of the phenomenon and master the process so that physicians will be able to induce it every time a tumor gets irradiated.