 Recent studies presented at the 2014 annual meeting of the American Society of Clinical Oncology (ASCO) indicate that checkpoint inhibitors used as a combination therapy can become the future for remission of advanced lung cancer.
Recent studies presented at the 2014 annual meeting of the American Society of Clinical Oncology (ASCO) indicate that checkpoint inhibitors used as a combination therapy can become the future for remission of advanced lung cancer.
According to the presentations at ASCO, it seems that immunotherapy is transforming treatment approaches to lung cancer. However, the real challenge is to evolve from a few patient responses to a fully activated, efficient and reproducible T cell response.
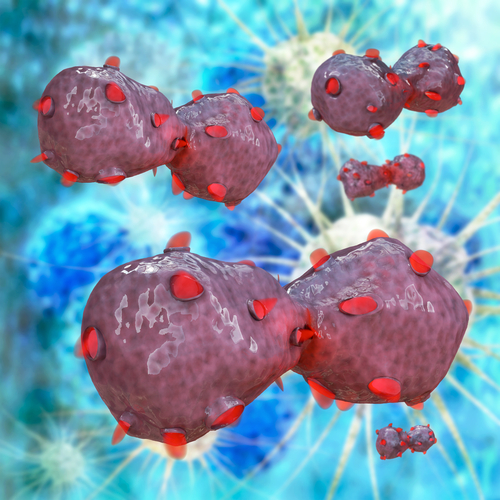
T lymphocytes display a potent anti-tumoral capacity, however, several coinhibitory and costimulatory ligands expressed at the surface of these cells are targeted by tumors to prevent them from recognizing and eliminating cancer cells.
Immune checkpoint inhibitors are designed to block these receptors, allowing T cells to maintain their cytotoxic potential. Even though several have already been identified, so far only two have been studied in clinical trials – PD-1/PD-L1 and CTLA-4– both demonstrating impressive results.
One of the studies presented at the meeting used nivolumab, an anti-PD1 monoclonal antibody, in patients with advanced lung cancer, observing a 20% overall survival after 2 years of treatment. Another study, presented by Edward B. Garon, MD, the director of the Medical Oncology Program in Thoracic Malignancies at the David Geffen School of Medicine at University of California, Los Angeles, used MK-3475, a selective PD-1 antibody in more than 200 patients with metastatic lung cancer, reaching objective response rates of 24% in patients known to express PD-L1 in their cancer cells. This experimental drug was characterized as tolerable inducing few toxic side effects.
MEDI4736, a human immunoglobulin G1 antibody preventing activation of PD-1 and CD80 receptors, was the focus of another study presented by Julie R. Brahmer, MD, an associate professor of oncology at Johns Hopkins University. The researchers reported that 24% of patients with non-small cell lung cancer (NSCLC) achieved a partial response, with only two patients showing a more modest tumor shrinkage.
In a third study, presented by Scott N. Gettinger, MD, an associate professor of medicine at Yale Cancer Center, New Haven, nivolumab administered in 50 patients with advanced NSCLC resulted in a 30% objective response rate and an 80% tumor bulk reduction in several patients, with PD-L1 expression correlating with response.
Even though these studies provide promising evidence regarding checkpoint inhibition in lung cancer, there is still a significant population who is not achieving a meaningful response either with multi-checkpoint blockade or with additional strategies stimulating T cell activity, such as vaccines or epigenetics.
“Treatments that increase T-cell infiltration to tumor sites are also going to increase PD-1 expression, and, therefore, anti-PD1 therapies provide the opportunity to enhance the net antitumor effect of other immunotherapies,” Drew M. Pardoll, MD, PhD, the director of cancer immunology at Johns Hopkins University School of Medicine, Baltimore, said in a Clinical Oncology interview.
Checkpoint inhibitors are seen as the future in the treatment of lung cancer, especially with the development of improved vectors and antigens. However immunotherapy is dependent on the capacity to address several signaling pathways, and is likely to be efficient only upon combination with other types of treatment, and not as a monotherapy.
“We are looking at some very exciting opportunities to move forward in the treatment of lung cancer. There is solid evidence that immunotherapy is effective, however we still have a lot of landscape to cover” added Dr. Pardoll in the same interview.