 A way to treat the number one cancer type in children? It may be possible, thanks to a collaboration among researchers at Children’s Hospital Los Angeles and MD Anderson Cancer Center. Writing in the journal Leukemia, the team is using autologous natural killer (NK) cells to battle acute lymphoblastic leukemia (ALL).
A way to treat the number one cancer type in children? It may be possible, thanks to a collaboration among researchers at Children’s Hospital Los Angeles and MD Anderson Cancer Center. Writing in the journal Leukemia, the team is using autologous natural killer (NK) cells to battle acute lymphoblastic leukemia (ALL).
“In this study, we used NK cells and ALL cells from the same pediatric patients,” explained Nora Heisterkamp, PhD, co-lead investigator of the study at Children’s Hospital, in a news story from Herald Online.
Although the work, published as “Cytotoxicity of CD56-positive Lymphocytes Against Autologous B-cell Precursor Acute Lymphoblastic Leukemia Cells” in Nature is currently on the bench top and not yet ready for human studies, the developing therapy has great promise. “We anticipate additional pre-clinical testing and then a clinical trial to evaluate the therapy in children with leukemia,” said Hisham Abdel-Azim, MD, another co-lead investigator of the study at Children’s Hospital. “These results are very promising–with potential as a part of first line therapy and also as a treatment for eliminating any remaining cancer cells, known as minimal residual disease, following standard chemotherapy.”
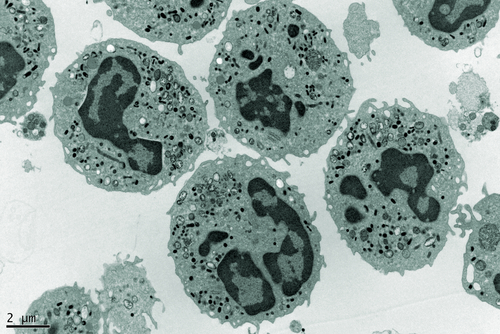
Currently, children with ALL must undergo two or three years of chemotherapy, putting them at risk for abnormal development and future infertility. The research team is aiming to provide a less toxic, more effective treatment known as immunotherapy. In essence, a patient’s own NK cells could be supercharged to fight cancer by destroying abnormal cells before they become cancerous.
“A patient’s own,” or autologous, is key to this NK cell immunotherapy due to the possibility of graft-versus-host disease if donor cells are used. However, multiplying leukemic patients’ NK cells to useful numbers was a problem that needed to be overcome: already, the number of NK cells in leukemic patients is depleted.
Despite any doubts, the research team selectively expanded NK cells from the bone marrow of patients while the cells were cultured along with cells decorated with the monoclonal antibody for BAFF-R. Heisterkamp’s laboratory previously showed that when this monoclonal antibody targets BAFF-R on the membrane of leukemia cells, NK cells are stimulated to attack the cancer cells.
This process enabled the NK cells to better identify leukemic cells as targets for destruction and neutralize foreign material. The cancer cells used in the study were also autologous, providing proof-of-concept that a patient’s own NK cells would be capable of killing that same patient’s cancer cells. Importantly, as stated by the article, “Since autologous cell therapy will not be complicated by graft-versus-host disease, our results show that expanded [NK cells] could be applied for treatment of pre-B-ALL without transplantation . . .”