 In a recent study titled “Harnessing the power of Vδ2 cells in cancer immunotherapy”, published ahead of print in the Clinical And Experimental Immunology journal, a group of researchers from St. George’s University of London discussed the available evidence on the potential of Vδ2 T cells to generate cytotoxic responses against tumors and assessed the current available immunotherapeutic approaches that target these cells in cancer patients.
In a recent study titled “Harnessing the power of Vδ2 cells in cancer immunotherapy”, published ahead of print in the Clinical And Experimental Immunology journal, a group of researchers from St. George’s University of London discussed the available evidence on the potential of Vδ2 T cells to generate cytotoxic responses against tumors and assessed the current available immunotherapeutic approaches that target these cells in cancer patients.
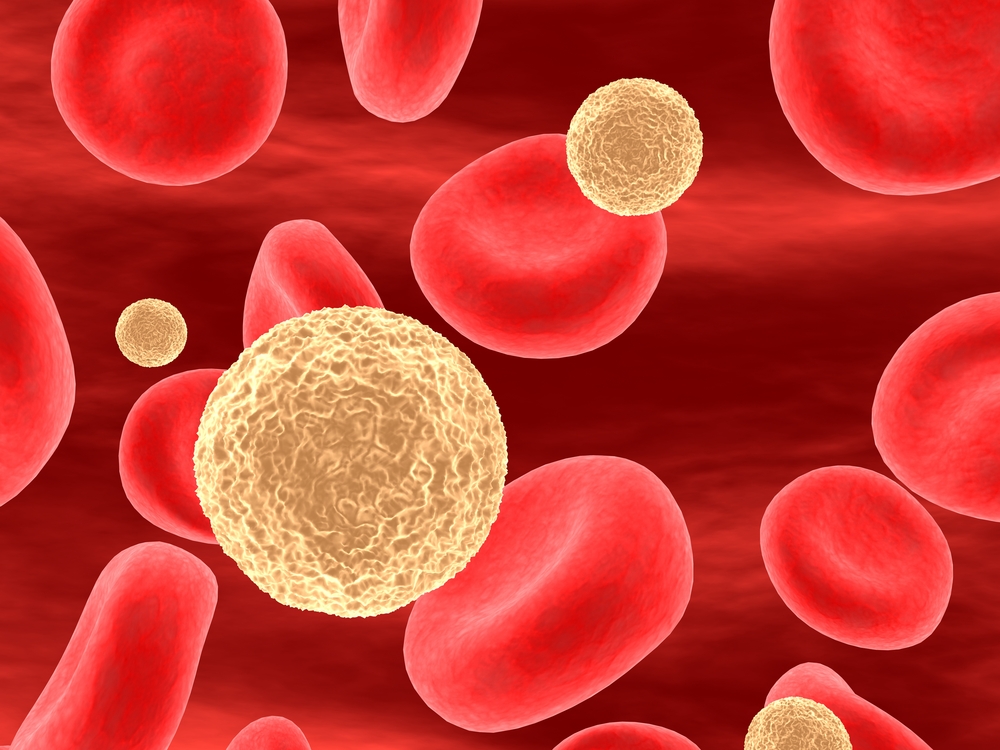
The most abundant (70-80%) and best characterized human γδ T cell subset expresses a Vg9Vd2 T cell receptor (TCR) and predominates in adult peripheral blood where it expands dramatically, from 2-10% up to over 50% of all perihperal blood lymphocytes upon infection. In other tissues, gd T cells mostly express TCRs composed of Vd1 or Vd3 regions, paired with a diverse array of Vg regions. Vd2 and non-Vd2 subsets differ in many different aspects.
Vd2 T cell activation is tightly regulated by many activating or inhibitor receptors, specificly for constitutively expressed or stress-modulated ligands. These cells are activated by different pathogens, through the action of non-peptidic products, namely phosphoantigens, such as hydroxymethylbut-2-enyl pyrophosphate (HMBPP), a metabolic intermediate specific to many prokaryotes and apicomplexan parasites.
The involvement of gd T cells in different physiopathological processes is reflected in their wide array of effector functions. They can kill infected, activated or transformed cells, through pathways involving the engagement of death-inducing receptors, such as FAS, and TNF-related apoptosis-inducing ligand receptors (TRAILR); they can also release cytotoxic effector molecules, such as perforin and granzymes, which are usually responsible for the clearance of tumor cells. In fact, human gd T cells are known to kill a vast repertoire of tumor cell lines and primary samples in vitro, such as leukemia and lymphoma, melanoma, neuroblastoma and several different types of carcinoma.
This type of T cells has increasingly gained attention in the field of immunotherapy. So far, two main approaches have been employed, either targeting Vδ2 cells in situ via intravenous (i.v.) administration of synthetic drugs called nitrogen-containing bisphosphonates (NBPs) or through adoptive transfer of in vitro-primed Vδ2 cells.
Both of these techniques have yielded encouraging results, however, there are still limitations that need to be overcome to improve their efficiency.
Some studies have shown that attenuated preparation of Mycobacterium bovis Bacillus Calmette Guérin (BCG) was capable of inducing clinical responses upon intravesicularly administration in bladder cancer, and could potentially be used upon intradermally injection in cancers such as melanoma.
Another approach towards Vδ2-based cancer immunotherapy includes adoptive transfer of in vitro-expanded populations of Vδ2 cells, which has already been tested in early phase clinical trials in breast cancer, lung cancer, metastatic melanoma and renal cell cancer.
“There is a growing body of in vitro data that supports the notion that Vδ2 cells can exert potent responses against tumour. Moreover, initial clinical evaluations of therapies specifically aimed at boosting Vδ2 cell anti-tumour immunity have supported this approach to cancer immunotherapy. (…) Further research into these areas will enhance the progression of Vδ2 cell immunotherapy and enable us to effectively prime the migratory and cytotoxic capacity of peripheral blood Vδ2 cells, whilst simultaneously increasing tumour susceptibility to Vδ2 killing”, the authors conclude in their study.