 A new cellular technology from Cell Source, an immunotherapy company, is being studied by researchers for the treatment of blood cancer and bone marrow transplantation.
A new cellular technology from Cell Source, an immunotherapy company, is being studied by researchers for the treatment of blood cancer and bone marrow transplantation.
Veto Cell technology, or T Central Memory Veto Cell technology, has the capacity to specifically fine-tune immune responses. It was first discovered when Professor Yair Reisner and colleagues at the Weitzman Institute of Science in Rehovot, Israel, found a particular cell that allowed immune responses to tolerate foreign antigens, such as crucial transplants, while still rejecting unwanted pathogens.
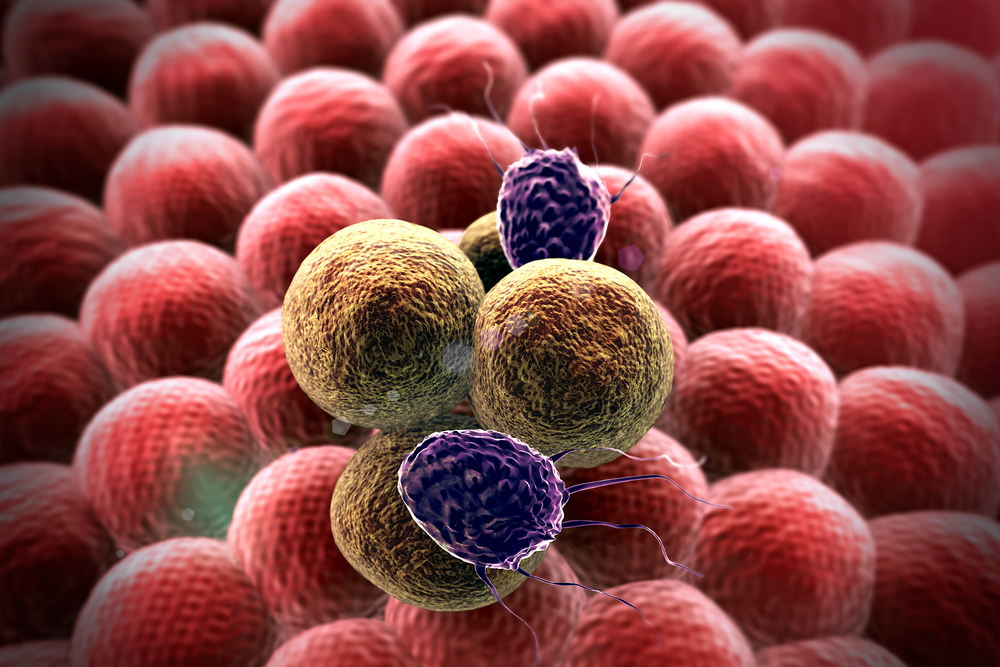
This technology platform can locate and kill lymphoma, leukemia and multiple myeloma cells. It acts as a trap by attracting the T cell clones that the patient immune system sends to attack donor cells. Once the T cell clones reach it, the veto cell can kill them and continue to live, travelling throughout the body killing only cancer cells until the disease is eliminated. This ultimately provides tumor clearance for patients who suffer from these types of malignancies.
The most potent known veto cells are activated CD8+ T cells, and its mechanisms of action include ligation of MHCI on the deleted cell by CD8 on the veto cell, Fas/FasL pathways and perforin action.
Veto cell can also be safely used to prevent organ rejection, avoiding the use of immunosuppressant drugs that compromise the patient’s immune system, allowing opportunistic pathogenic infections.
This technology can disable the immune attack on the healthy transplant without jeopardizing the patient’s immune system. This can hopefully allow improved bone marrow transplantation (BMT) to treat a larger number of blood cancers.
Furthermore, Veto cell can be used in combination with an approved FDA cell therapy, allowing the use of mismatched BMT and increasing the overall survival rates associated with transplantation.
In addition to this technology, Cell Source is also developing Organsource, an innovative method for growing and healing human organs, such as pancreas and liver, using pig embryonic tissue.
Previous experiments have already successfully managed to grow a mouse pancreas and a primate pancreas within the body of its carrier, to efficiently treat diabetes.