 During the 56th Annual Meeting of the American Society of Hematology (ASH) conference in San Francisco, researchers from the University of Texas MD Anderson Cancer Center presented their latest clinical trials’ results whereby CD19-directed chimeric antigen receptor (CAR) therapy using the Sleeping Beauty non-viral transduction system to modify T cells was successfully used in the treatment of patients suffering from advanced forms of blood cancers.
During the 56th Annual Meeting of the American Society of Hematology (ASH) conference in San Francisco, researchers from the University of Texas MD Anderson Cancer Center presented their latest clinical trials’ results whereby CD19-directed chimeric antigen receptor (CAR) therapy using the Sleeping Beauty non-viral transduction system to modify T cells was successfully used in the treatment of patients suffering from advanced forms of blood cancers.
“We are treating patients with advanced CD19 positive hematologic malignancies using CAR T cells in combination with conventional blood stem cell transplantation,” said Partow Kebriaei, M.D., associate professor of stem cell transplantation and cellular therapy, who along with Laurence Cooper, M.D., Ph.D., professor of pediatrics developed the study published in Blood. “We are also treating patients who had active disease but had not received blood stem cell transplantation.”
The gene was called Sleeping Beauty since it has the capacity to activate, or “awaken” an extinct piece of DNA (transposon) that can multiply and become inserted into the genome. This allows researchers to use a gene in a piece of DNA known as plasmid. After that, an enzyme (transposase) can take out the gene of interest from the plasmid and insert it into the targeted DNA sequence.
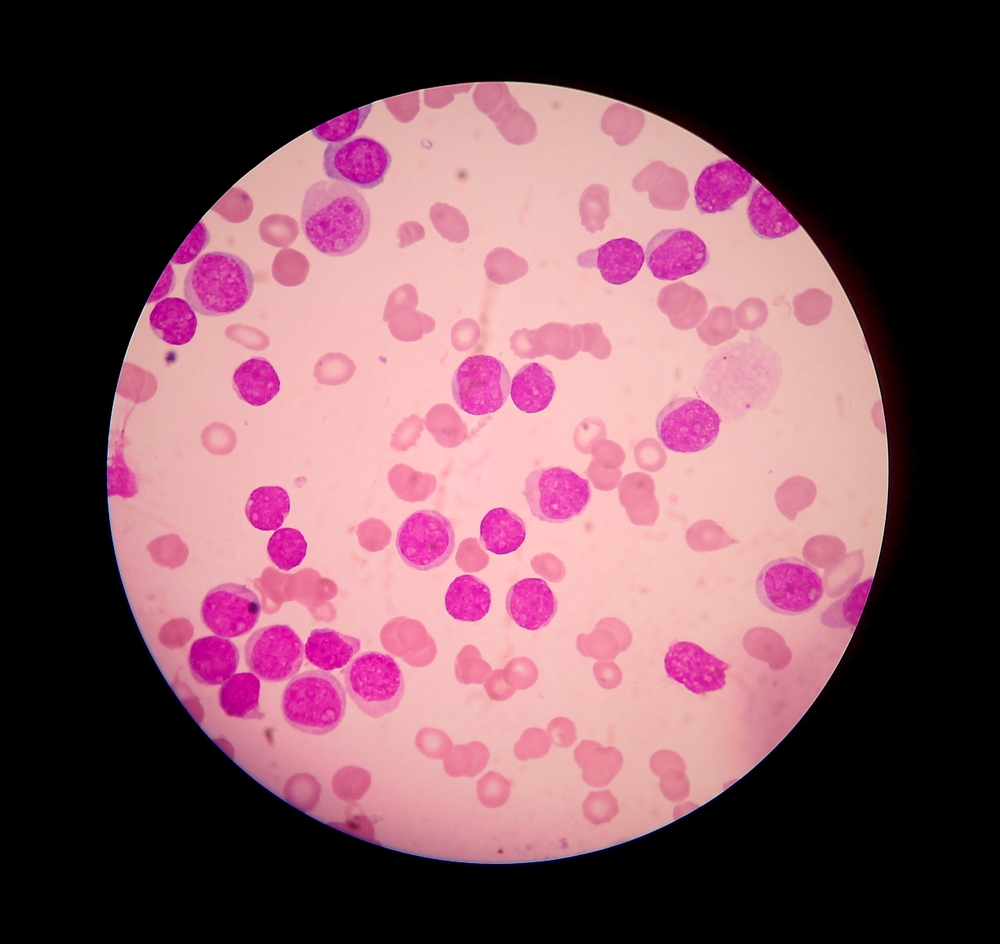
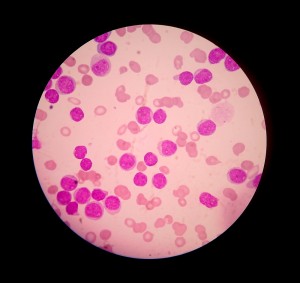
During the study, the team assessed patients diagnosed with acute lymphocytic leukemia (ALL), non-Hodgkin lymphoma (NHL) and chronic lymphocytic leukemia (CLL), and used the Sleeping Beauty transfer system to insert a gene into T cells, resulting in a chimeric antigen receptor (CAR) that has the capacity to bind to the CD19 receptor present on the surface of B cells.
The patients who participated in the trials received either their own cells or donor stem cell transplantation, alongside with CAR administration.
No severe of long-term toxicity was verified in any of the 33 patients treated. “Five patients at high risk for relapse were treated with CAR T cells along with autologous stem cell transplant, and four of those patients remain in complete remission with a median follow-up of 12 months,” Dr. Kebriaei added. “Among 13 patients treated with donor CAR T cells after allogeneic stem cell transplantation, six remain in complete remission with a median follow-up of 7.5 months.”
Importantly, 5 out of 14 patients who received CAR T cells and did not receive blood stem cell transplantation, exhibited disease regression with a median follow-up of six months.
This study was funded by the National Institutes of Health and the Cancer Prevention and Research Institute of Texas and continues to be developed under MD Anderson’s Moon Shots Program.