 In a new study published in the Journal of Clinical Investigation, a research team from the Children’s Hospital Los Angeles (CHLA) designed a new protein-based therapy that may be extremely efficient against drug-resistant leukemia cells. Importantly, this protein fusion also has the potential to enhance the efficacy of commonly used treatments such as chemotherapy and radiation therapy.
In a new study published in the Journal of Clinical Investigation, a research team from the Children’s Hospital Los Angeles (CHLA) designed a new protein-based therapy that may be extremely efficient against drug-resistant leukemia cells. Importantly, this protein fusion also has the potential to enhance the efficacy of commonly used treatments such as chemotherapy and radiation therapy.
One of the most common problems in the treatment of acute lymphoblastic leukemia (ALL) is the resistance of cancer cells to current chemotherapeutic drugs. In this study, the authors assessed the efficiency and safety profile of a novel fusion protein, using animal models transplanted with aggressive human ALL cells.
“Despite advances in available therapies, unmet and urgent needs remain in the fight against leukemia. We still have children with disease that our drugs can’t help enough. And for patients who relapse, their chances of long-term survival are less than 20 percent. We’ve got to do better”, study’s principal investigator, Fatih M. Uckun, MD, PhD, of the Children’s Center for Cancer and Blood Disease at CHLA and the Norris Comprehensive Cancer Center of the University of Southern California (USC), said in a news release.
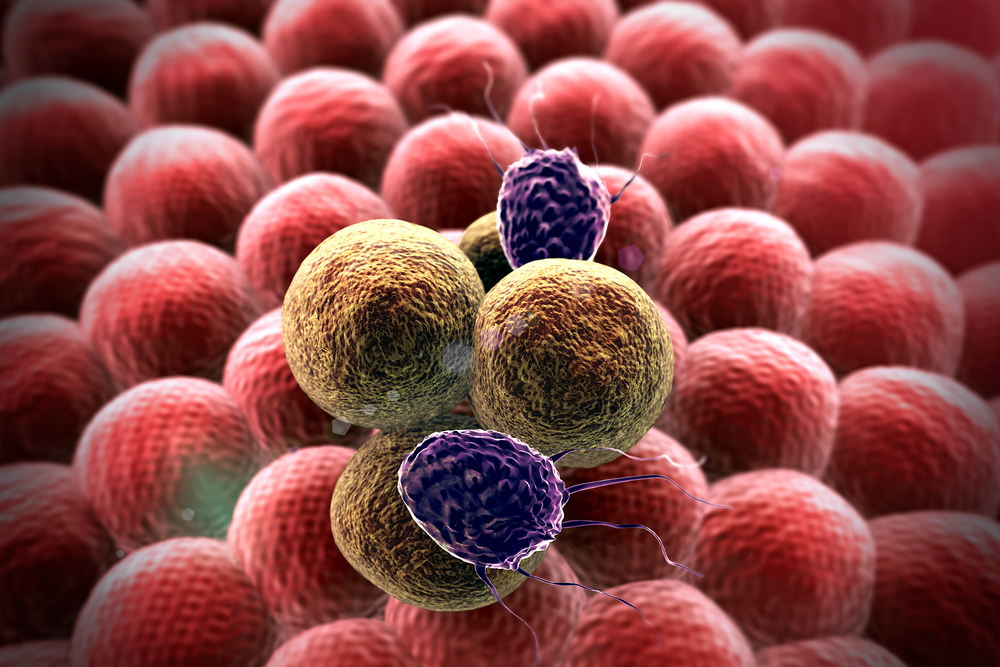
TNF-related apoptosis-inducing ligand (TRAIL) is a protein present in different cells from the immune system, whose function includes the induction of cellular apoptosis (cell death). As such, upon binding with its receptors (TRAIL-receptor 1 and 2) present in tumor cells, a cascade of signaling events is initiated, ultimately resulting in tumor cell death.
“TRAIL is a naturally occurring part of the body’s immune system that kills cancer cells without toxicity to normal cells. However, earlier clinical trials using TRAIL as a potential anti-cancer medicine candidate have not been successful, largely because of its propensity to bind, not only to cancer cells, but also to ‘decoy’ receptors,” Dr. Uckun explained in the news release.
The team identified a protein called CD19 ligand, which can bind to a receptor present in the majority of human ALL cells. They then fused it with part of the TRAIL protein, producing a powerful weapon against these cancer cells. The novel fusion protein was named CD19L-sTRAIL, and showed a highly efficient capacity to trigger apoptosis, even in the most aggressive forms of therapy resistant leukemia cells.
“Due to its ability to anchor to the surface of cancer cells via CD19, CD19L-sTRAIL was 100,000-fold more potent than sTRAIL, and consistently killed more than 99 percent of aggressive leukemia cells taken directly from children with ALL – not only in the test tube, but also in mice,” said Dr. Uckun. “The biggest challenge is to cure patients who experience a recurrence of their cancer, despite intensive chemotherapy. We are hopeful that the knowledge gained from this study will open a new range of effective treatment opportunities for children with recurrent leukemia”, he concluded.