 In a recent press release, cancer experts Rhoda M. Alani, MD, FAAD, Herbert Mescon, dermatologist-in-chief at Boston Medical Center; and Debjani Sahni, MD, assistant professor of dermatology and director of the cutaneous oncology program at Boston University School of Medicine highlighted the major advancements in targeted therapy and immunotherapy treatments for advanced melanoma patients.
In a recent press release, cancer experts Rhoda M. Alani, MD, FAAD, Herbert Mescon, dermatologist-in-chief at Boston Medical Center; and Debjani Sahni, MD, assistant professor of dermatology and director of the cutaneous oncology program at Boston University School of Medicine highlighted the major advancements in targeted therapy and immunotherapy treatments for advanced melanoma patients.
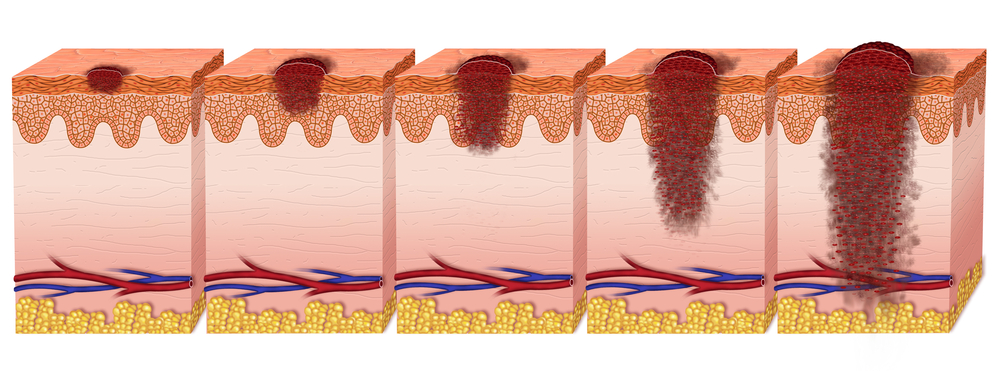
While melanoma is still the deadliest of skin cancers (responsible for 75% of all skin cancer deaths) if detected early (stage I), patients’ survival rates at five years is of 98%, making early detection the most effective way of preventing melanoma. Accordingly, the American Academy of Dermatology highlights the need for regular skin self-exams to identify any skin change that might be undergoing along with the importance of consulting a board-certified dermatologist.
However, in advanced stages, patients’ survival rates decrease to 63% and 16% when cancer cells are able to reach lymph nodes and metastasize to nearby organs or distant organs, respectively. Melanoma research and pharmaceutical industries, however, have developed new drugs specifically focused on advanced melanoma patients.
Targeted therapies were developed to target BRAF mutations, a genetic defect frequently detected in melanomas, more than 50% of which (one of such mutations, BRAFV600E is actually observed in 90% of all melanoma cases) underlies melanomagenesis, mostly by deregulating the activity of downstream MEK/ERK effectors. Since cancer cells when treated with BRAF inhibitors (drugs that induce tumor shrinking in patients with BRAF mutations) may develop resistance to the drug, an additional targeted therapy was developed: MEK inhibitors targeting the same pathway but a different protein.
Currently, targeted therapy is given to patients as a combination of both BRAF inhibitors and MEK inhibitors to provide a more effective way to prevent treatment resistance in advanced melanoma patients. Of note, the combination of both drugs decreases treatment adverse effects, thus proving a safer option for patients.
Another strategy to fight advanced melanoma relies on immunotherapies, i.e., a treatment that uses patients’ own immune system to attack cancer cells. While the immune system usually has molecules (called “checkpoints”) that act like a switch to turn the immune system on or off, drugs targeting these immune “checkpoints” can turn them on and initiate an immune response directed towards melanoma cancer cells. Currently, examples of these drugs include PD-1 inhibitors or CTLA-4 inhibitors.
As with targeted therapies, combined immune-therapies harbor the promise of an enhanced immune response and consequently increased treatment efficacy. Thus, cancer experts emphasize that the future of melanoma therapy resides on combined and personalized therapies, where each patient will receive the most appropriate and effective combinatory-therapy for their cancer characteristics.
As Dr. Sahni noted in the press release, “Four years ago, we had nothing to improve advanced melanoma patients’ survival, and now we have several new therapies available, with several others in the pipeline. Although these developments are promising for patients, we don’t have all the answers yet. There’s a lot more research that needs to be done. This is a really exciting time for melanoma therapy. We’re doing all we can to make a dent in this disease. However, early detection is still vital. The sooner that melanoma is found and treated, the better the patient’s chance of survival will be.”