 In a new study entitled “Improved anti tumor activity of immunotherapy with BRAF and MEK inhibitors in BRAFV600E melanoma,” researchers show increased anti-tumor activity of a triple therapy – BRAF and MEK inhibitors with immunotherapy — in BRAF mutant melanoma. The study was published in the journal Science Translational Medicine.
In a new study entitled “Improved anti tumor activity of immunotherapy with BRAF and MEK inhibitors in BRAFV600E melanoma,” researchers show increased anti-tumor activity of a triple therapy – BRAF and MEK inhibitors with immunotherapy — in BRAF mutant melanoma. The study was published in the journal Science Translational Medicine.
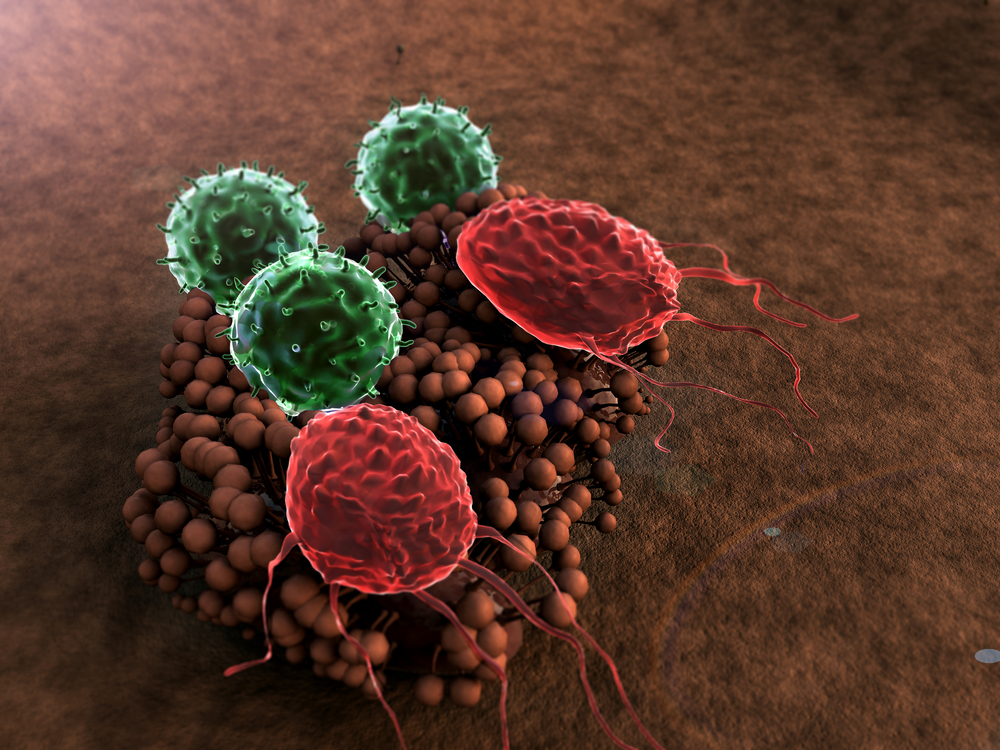
Advanced melanoma, characterized by a stage where cancer cells reach lymph nodes and can therefore metastasize in nearby and distant organs, is diagnosed in 70,000 patients every year in the United States alone.
Current therapeutics rely on BRAF inhibitors and/or MEK (MAPK [mitogen-activated protein kinase]) inhibitors to fight tumors, since 50% of melanoma patients harbor BRAF mutations. BRAF genes regulate the MAPK pathway, responsible for cell growth, proliferation, and differentiation and thus BRAF mutations allow tumor cells to become more proliferative and resistant to apoptosis (programmed cell death). Combining targeted therapies (as with BRAF inhibitors or MEK inhibitors) with immunotherapy (a strategy devised to elicit or amplify an immune response) promises to increase anti-tumor responses. However, the first clinical trial that combined targeted and immunotherapy resulted in severe liver toxicity.
In this study, a team of researchers at UCLAs’ Jonsson Comprehensive Cancer Center developed a new and more effective treatment against melanoma by combining immunotherapy with a BRAF inhibitor (dabrafenib) and MEK inhibitor (trametinib). The authors used a syngeneic (i.e., genetically identical) BRAFV600E mutant (the most common BRAF mutation) melanoma mouse model and showed that adding a MEK inhibitor increased the anti-tumor activity of immunotherapy with dabrafenib. Specifically, the authors found the triple strategy resulted in tumor regression and higher penetration of immune cells targeted against the tumor, decreasing in vivo cytotoxicity.
The team highlighted that the triple therapy – BRAF and MEK inhibitors with immunotherapy — is a potential new treatment for patients with BRAFV600E metastatic melanoma.
Dr. Antoni Ribas, Professor of Hematology and Oncology at UCLA and study lead author commented in a press release, “The two drug combination of BRAF and MEK inhibitors works synergistically and decreases the side effects of the BRAF inhibitor or normal cells. We reasoned that this combo would allow us to synergize with immunotherapy without increasing toxicities. We have made incredible progress in the last three years of treating advanced melanoma, with six new drug therapies approved by the FDA. Half are immunotherapies and the other half are BRAF or MEK inhibitors. The next step is to figure out how to rationally combine them and merge their benefits in the clinic.”
Hu-Lieskovan, the study’s first author and clinical instructor of Hematology and Oncology at UCLA added, “The triple combination of targeted therapies BRAF (dabrafinib) and MEK (trametinib) inhibitors with immunotherapy (tumor antigen-specific adoptive cell transfer or anti-PD1 antibody) makes immune therapy more effective at killing cancerous tumors and causes less toxicity. We’re trying to take advantage of the high response rate of the targeted therapy and durability of the immune therapy to induce a response that lasts in the majority of patients.”