In a new study entitled “Noninvasive imaging of immune responses,” researchers at the Whitehead Institute for Biomedical Research used positron emission tomography (PET) imaging to detect anti-tumor immune responses. This technique promises a new way to monitor anti-cancer therapies in patients without the necessity of blood analysis or biopsies. The study was published in the journal Proceedings of the National Academy of Sciences (PNAS).
Immune cells, such as neutrophils, dendritic cells and macrophages, usually surround tumors. These cells, once activated, express markers, such as the class II MHC and CD11b. In this study, researchers at the Whitehead Institute postulated that tracking immune cells’ interaction with tumor and stroma cells could be used to monitor the immune responses triggered in anti-cancer therapies and therefore assess patients’ responses without the need for invasive methods, such as biopsies.
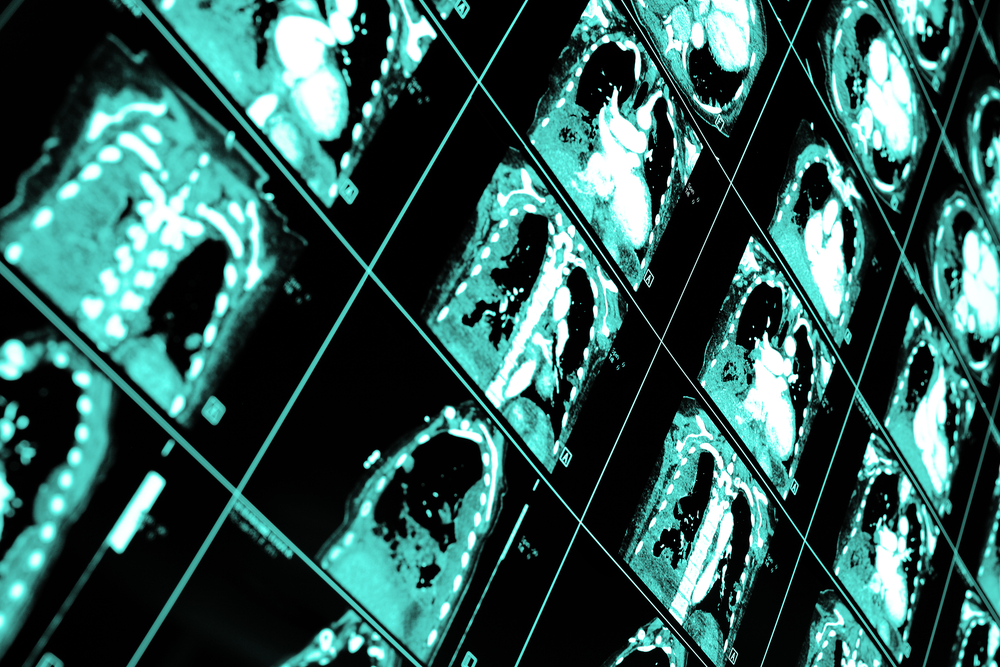
The team, led by Dr. Hidde Ploegh, took advantage of the laboratory expertise with single-domain antibodies known as VHHs and sortagging (sortase-mediated transpeptidation, where small probes are used to label proteins at specific sites) to produce alpaca-derived antibody fragments that specifically target mouse class II MHC and CD11b markers, found at the surface of several immune cells. The labeled cells were injected back into tumor-bearing mice and subsequently analyzed by positron emission tomography (PET). The team observed that the radiolabeled-VHHs were rapidly detected in tumors with high specificity.
Mohammad Rashidian, study first author and a postdoctoral researcher in Ploegh’s lab noted, “We were able to image tumors as small as one millimeter in size and within just a few days of their starting to grow. We’re very excited about this because it’s a powerful approach to pick up inflammation in and around the tumor.”
The team hopes that with further work and due to the easy production and labeling of VHHs, this method can revolutionize how cancer immunotherapies are monitored in patients.
“To succeed with immunotherapy, we need more information about the tumor microenvironment. With this method, you could perhaps start immunotherapy, and then, a few weeks later, image with VHHs to figure out progress and success of treatment,” commented Rashidian.
Ploegh added, “PET imaging should allow a much more comprehensive look at the entire tumor in its environment. Then we can ask, ‘Did the tumor grow? Did immune cells invade? What has happened to the tumor?’ And to be able to see this without going in invasively is a significant achievement.”