In a new study entitled “Nivolumab versus Docetaxel in Advanced Squamous-Cell Non–Small-Cell Lung Cancer” researchers show that patients with squamous-non-small cell lung cancer live for longer periods of time (3.2 months) when treated with nivolumab, an immunotherapeutic drug, when compared to patients treated with chemotherapy. The study was published in the New England Journal of Medicine.
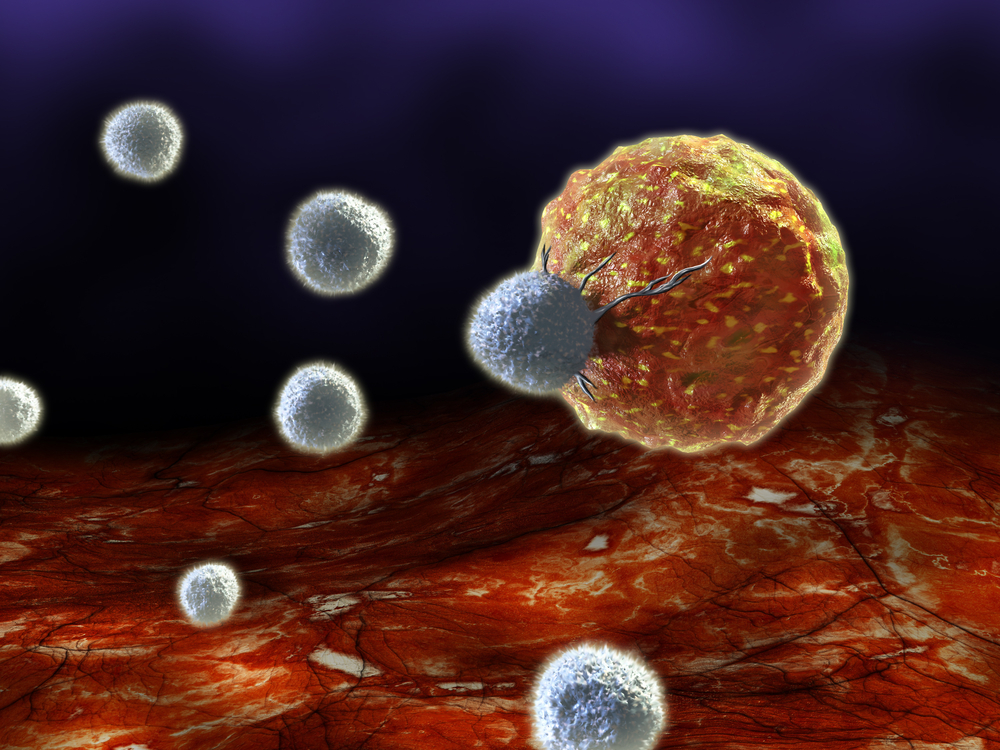
Researchers designed a randomized, open-label, international, phase 3 clinical trial enrolling patients with advanced squamous-cell non–small-cell lung cancer (NSCLC) who received chemotherapy but whose disease continued to progress. Specifically, the study aimed to evaluate the efficacy and safety of nivolumab, a human antibody that belongs to the class of “checkpoint inhibitor” drugs. Specifically, nivolumab is a fully human programmed death 1 (PD-1) immune checkpoint inhibitor antibody, i.e., it inhibits the expression of the PD-1 receptor in immune T cells allowing them to restore an anti-tumor immune response.
In this new trial, 272 patients were randomly assigned to receive nivolumab (3 mg per kilogram of body weight every 2 weeks) or docetaxel, a clinically well-established chemotherapy medication during 3 weeks. Researchers observed that while patients under chemotherapy had a median overall survival (OS) of 6 months, those treated with nivolumab had an OS of 9.2 months. At one year, 42% of nivolumab treated patients remained alive, while the survival decreased for 24% in patients taking docetaxel. Treatment response was significantly higher with nivolumab (20%) when compared to the chemotherapy group (8.8%). Moreover, the median disease-progression free survival was of 3.5 months and 2.8 months, for nivolumab and docetaxel, respectively; the relative risk of dying from lung cancer was reduced to 41 percent with nivolumab when compared with docetaxel.
Thus, as noted by Julie Brahmer, M.D., director of the Thoracic Oncology Program at the Johns Hopkins Kimmel Cancer Center and study first author “This solidifies immunotherapy as a treatment option in lung cancer. In the 20 years that I’ve been in practice, I consider this a major milestone.” She added, that while “Immunotherapy can produce severe side effects, and it’s important to be vigilant in efforts to manage them. However, it is less toxic than chemotherapy.”
The results in median survival time are somehow misleading since, “Patients who respond to immunotherapy tend to continue their responses for long durations, and these lengthier responses are cut off in calculations of median overall survival,” commented Brahmer. Thus, one- and two-year survival data will indicate with more accuracy the positive benefits in patients survival.