Researchers at the Tisch Cancer Institute at the Icahn School of Medicine at Mount Sinai revealed a new mechanism by which radiotherapy can successfully eradicate melanoma. These findings were published in Nature Immunology in a study entitled “CDKN1A regulates Langerhans cell survival and promotes Treg cell generation upon exposure to ionizing irradiation.”
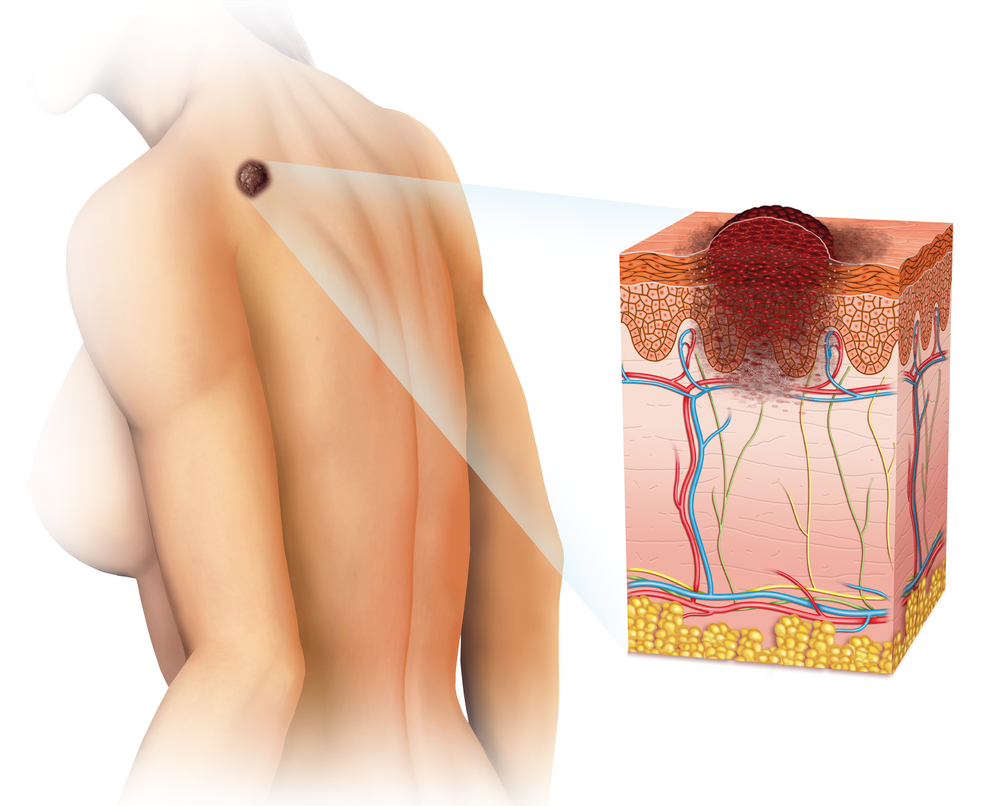
Ionizing radiation is a potent therapeutic strategy to damage cellular DNA and has been used to treated several types of cancer, including melanoma. In this study, researchers found that Langerhans cells (LCs), skin immune cells localized in the basal and suprabasal layers of the epidermis, are activated during radiotherapy in skin tumors, becoming resistant to apoptosis, i.e. cell death, and rapidly repairing DNA damage after exposure to ionizing radiation, i.e. radiotherapy, in mouse models of melanoma. Notably, these cells were still able to acquire antigens in the skin and transport them to nearby lymph nodes to interact with regulatory T (Treg) cell (cells that suppress the immune system), which then return to the tumor site, protecting it from further attacks of the immune system.
Researchers used an approach similar to immunotherapy drugs called “immune checkpoint inhibitors” to enhance the immune action against tumors. This strategy inhibited Langerhans cells to repair their own DNA after radiotherapy, resulting in cellular death and preventing tumor protection. Specifically, researchers found that a protein called cyclin-dependent kinase inhibitor CDKN1A (p21) was overexpressed in wild-type LCs and that LCs deficient for Cdkn1a underwent apoptosis and accumulated DNA damage after radiotherapy. Moreover, LCs deficient for the Cdkn1a gene did not activate Treg after radiotherapy and protected skin tumors from further ionizing radiation.
“Our study suggests that this combination approach — combining radiotherapy with drugs that rev up a healthy immune response — will help make radiation therapy much more effective,” study’s lead author, immunologist Jeremy Price, PhD, said in a press release.
“Similarly, checkpoint-inhibiting drugs have revolutionized the treatment of melanoma and are being investigated in many other cancers,” said co-author Miriam Merad, MD, PhD, Professor of Tumor Immunology, Oncological Sciences, and Hematology and Medical Oncology at The Tisch Cancer Institute at the Icahn School of Medicine at Mount Sinai. “Cancer has the ability to turn off and even evade the body’s natural immune response to tumors — the new immunotherapy drugs take the brakes off the immune system, promoting a powerful and complete immune response to the cancer.”
The authors believe that tumors’ capacity to switch-off and escape the immune system can be overcome by novel immunotherapeutic drugs, through induction of a potent and complete immune response against tumors. “This is synergized by the addition of radiation, which can expose the tumor so it can better be targeted by the immune system,” said Dr. Price. “By combining these treatments, the ability of Langerhans cells to use the immune system to protect cancers will be overwhelmed,” he added.
“We found melanoma grew much more quickly on mice pretreated with radiation, compared to untreated mice, because of the presence of regulatory T cells activated by Langerhans cells,” Dr. Price further explained. “These Langerhans cells were resistant to radiation.”
“Any treatment that prevents tumor infiltrating regulatory T cells from being produced, such as immunotherapy, will improve the outcome from radiation treatment — and that will save lives,” Dr. Price concluded.