Researchers at Philadelphia’s Wistar Institute investigating the effects of tumor-targeted therapies on the immune system found that many of these agents, such as FDA-approved trametinib, actually suppress the activity of cancer-fighting T-cells.
However, researchers also found that these suppressing effects can also be weakened by certain cytokines, such as IL-15, while also preserving the therapies’ cancer-blocking effects. The research paper, “IL-15 Agonists Overcome the Immunosuppressive Effects of MEK Inhbitors,” was published in Cancer Research.
Targeted cancer therapies rely on the attack of cancer cells that present specific tumor-promoting mutations, while preserving healthy, normal cells. This mechanism has made these treatments preferable to other therapeutic strategies such as chemotherapy and radiation therapy.
The effect of targeted therapies on tumor cells have been studied and described in several clinical trials, but their effect on the immune system remains poorly understood, despite the fact that the targeted pathways may also be important for the function of anti-cancer lymphocytes.
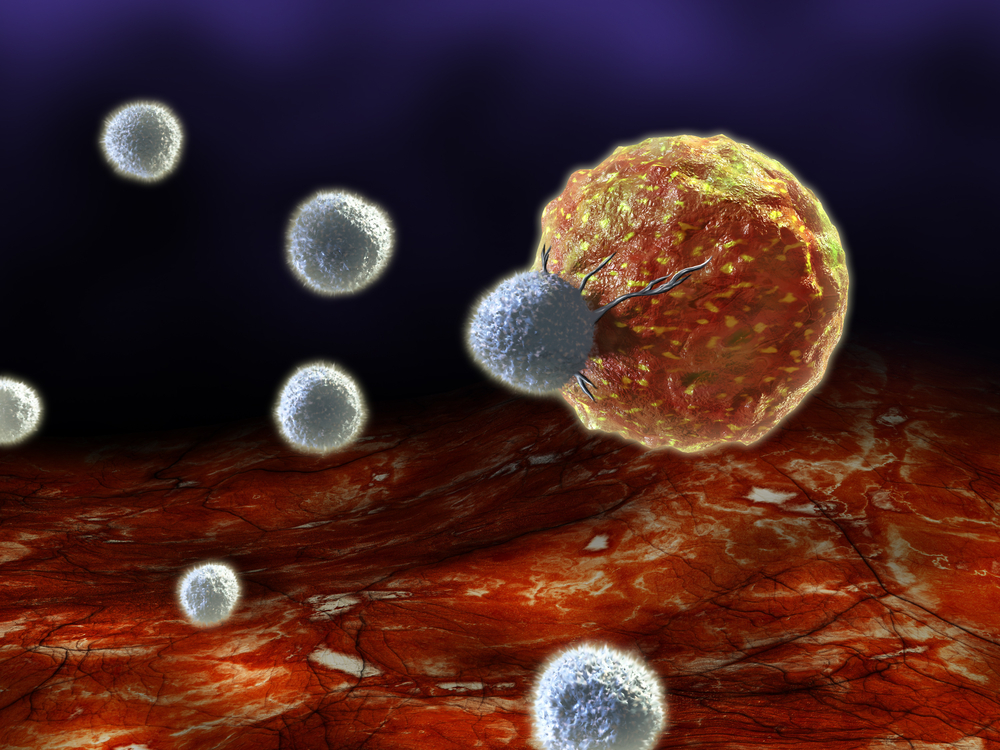
Researchers investigated 41 targeted therapies and their effects on healthy human T-cells, essential for the body’s defense against cancer. The team found that each of these therapies inhibited T-cells in a more potent manner than they did cancer cells. This was especially powerful with trametinib (Mekinist), an MEK1/2 inhibitor approved to treat metastatic melanoma with a BRAFV600E/K mutation.
Researchers theorized that cytokines could rescue T-cells from the negative effects of trametinib treatment by promoting the signaling of the immune cells but not the tumor cells. After selecting interleukin-15 (IL-15) as a promising candidate, researchers tested an investigational IL-15 “superagonist,” ALT-803, for its T-cell rescue effects and found that, in vivo, this IL-15 agonist prevented T-cell attacks from trametinib.
“MEK inhibitors like trametinib are being tested in a variety of tumors, and we’ve demonstrated an effective means of controlling the effect that these drugs have on T-cells that could further help in the fight against cancer,” Michael Allegrezza, first author of the study, said in a news release. “We plan to continue to study the effects of targeted therapies on the tumor microenvironment and see if other immune cells are impacted in the manner we observed in effector T-cells.”