ITMO University of Russia researchers, joined by those at several U.S. universities, examined thousands of genome profiles from patients with lung adenocarcinoma and lung squamous cell carcinoma, the most common types of lung cancer, and identified a series of driver mutations that clearly distinguish the two types of cancer and provoke disease onset. They also found several different protein fragment markers that hold potential for new immunotherapies.
The study, “Distinct patterns of somatic genome alterations in lung adenocarcinomas and squamous cell carcinomas,” was published in Nature Genetics.
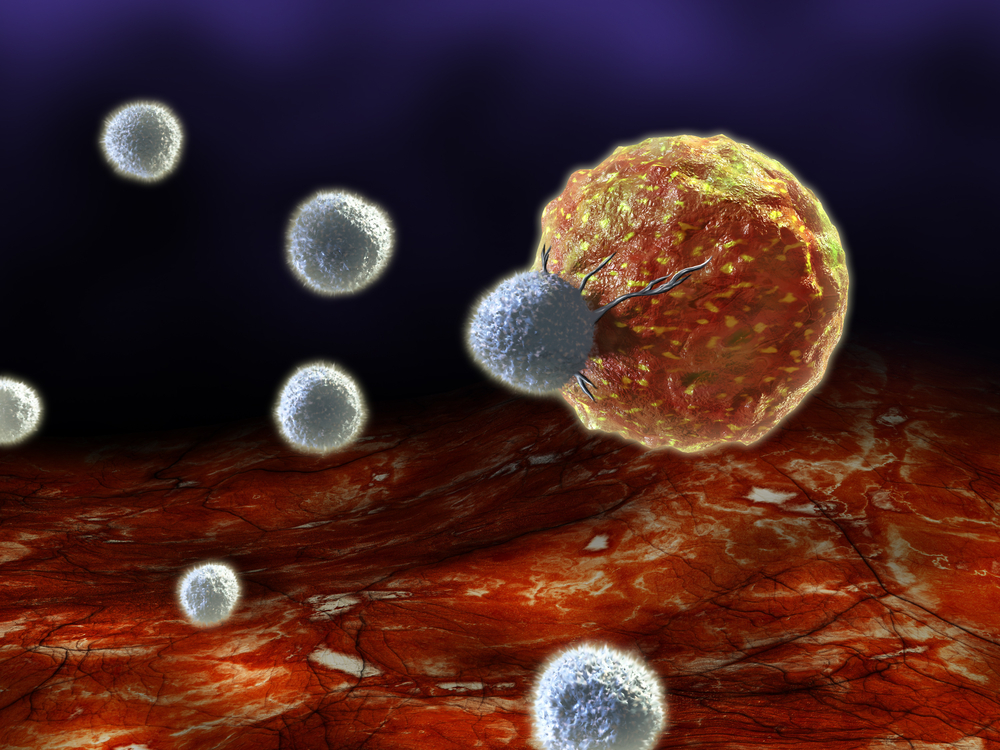
Immunotherapy is a treatment approach with promise, since unlike chemotherapy and radiotherapy it only targets tumor cells and leaves healthy cells unaffected. Cancer immunotherapy, in which the immune system is stimulated to fight malignant cells, has shown results in studies of many cancers. Several approaches consist in the targeting and inhibition of a variety of checkpoint receptors on the surface of T-cells, reactivating their capacity to target cancer cells.
Epitopes are protein fragments provided by cells that the immune system recognizes and uses to review, evaluate, and fight foreign pathogens or diseased cells. However, sometimes the immune system is unable to capture these markers, a failing that can lead to the development of cancer. Identification of cancer-related and patient-specific epitopes might lead to more accurate immune responses and, therefore, more effective treatments.
Researchers analyzed 1,144 genome profiles from patients with lung adenocarcinoma and lung squamous cell carcinoma, and identified 38 significantly mutated genes in lung adenocarcinoma and 20 in squamous cell carcinoma. Importantly, only six genes were common to both types of lung cancer, suggesting that these two forms are very distinct from each other. Moreover, researchers found that lung squamous cell carcinoma is more similar to head and neck tumors and to a subset of bladder carcinomas, than to lung adenocarcinomas.
Importantly, 47% of all lung adenocarcinomas and 53% of all lung squamous cell tumors had at least five predicted neoepitopes. “We have identified several distinct recurrent mutations that are likely to be recognized by the immune system and therefore would be strong candidates for cancer vaccines,” Dr. Joshua Campbell, the study’s lead author and a postdoctoral associate at Broad Institute of MIT and Harvard, said in a news release.
Researchers emphasize that, according to these results, cell type is a key factor to determine if the mutation will cause abnormal cell growth and lead to tumor development. “Future studies are needed to determine what allows a mutation in a gene to cause uncontrolled growth in one type of cell but not in another type. This knowledge will give us a more complete understanding of the molecular pathways involved in tumor growth and help us design better drugs,” Dr. Campbell concluded.