Modifying the identity of key immune cells found in tumors by targeting a specific protein, named Helios, was seen to enhance the cells’ anti-tumor activity in melanoma or colon mice models, and researchers plan to move the treatment into clinical testing in cancer patients. The findings were published in the Proceedings of the National Academy of Sciences, in the study “Instability of Helios-deficient Tregs is associated with conversion to a T-effector phenotype and enhanced antitumor immunity.”
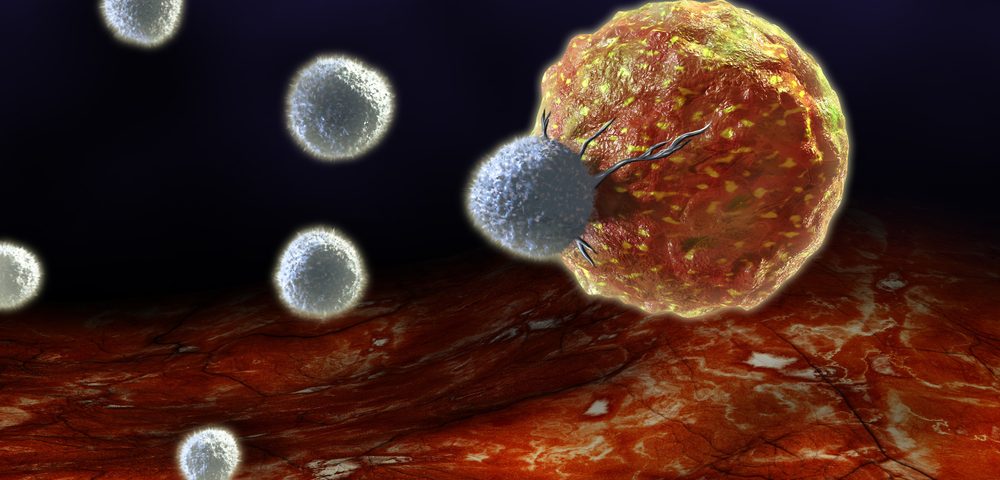
Regulatory T-cells (Tregs) are a subpopulation of T-cells known to modulate the immune system by suppressing induction and proliferation of effector T-cells (Teffs). Tregs are often increased in tumors where they suppress tumor immunity, inhibiting the body’s ability to control tumor growth. High levels of Tregs in both humans and animal models have been associated with poor prognosis, suggesting that modulation of Tregs can help treat cancer patients.
Previous research carried out by Harvey Cantor, MD, the Baruj Benacerraf Professor in the department of Cancer Immunology and Virology at the Dana-Farber Cancer Institute, and Hye-Jung Kim, PhD, lead scientist in the department of Cancer Immunology and Virology at Dana-Farber, and colleagues had shown that a specific protein called Helios was essential for Tregs to maintain their immune-suppressive properties under inflammatory conditions. Decreasing Helios levels in Tregs made them lose stability and change their identity into effector T-cells.
To understand whether this conversion into effector T-cells had therapeutic potential in cancer-cell targeting, the research team injected melanoma or colon cancer cells into mice genetically engineered to lack Helios in their Treg cells. These mice were found to develop tumors at a slower rate than mice with normal Tregs. “Inspection of the animals’ tumor tissue showed an unstable set of T regulatory cells, many of which had converted into Teffs,” Dr. Kim said in a press release.
In a second phase of the study, the scientists tested several antibodies that recognized receptors on the surface of Treg cells, and selected one that diminished Helios expression. Their results showed that the antibody also triggered the conversion of Tregs into effector T-cells.
“Many current approaches to immunotherapy involve depleting or blocking Tregs in order to shift the balance toward Teff cells,” Dr. Cantor said. “This, however, runs the risk of triggering an autoimmune response in which the Teff cells attack normal as well as malignant tissue. The key to our approach is that it singles out the Tregs inside a tumor for conversion, leaving Tregs elsewhere in the body unchanged.
“We now have a very specific, targeted way of inducing a T effector cell attack on cancer, while lowering the risk of adverse effects on healthy tissue. The next step will be to organize a clinical trial using this approach in patients,” he added.