A recent clinical study found that a combination immunotherapy using talimogene laherparepvec (T-VEC) plus ipilimumab is safe and effective in patients with untreated and unresectable advanced melanoma.
The study, “Talimogene Laherparepvec in Combination With Ipilimumab in Previously Untreated, Unresectable Stage IIIB-IV Melanoma,” was published in the Journal of Clinical Oncology.
When compared to monotherapy, the combination of two or more therapeutic agents has been shown in different studies to be more efficient in melanoma treatment.
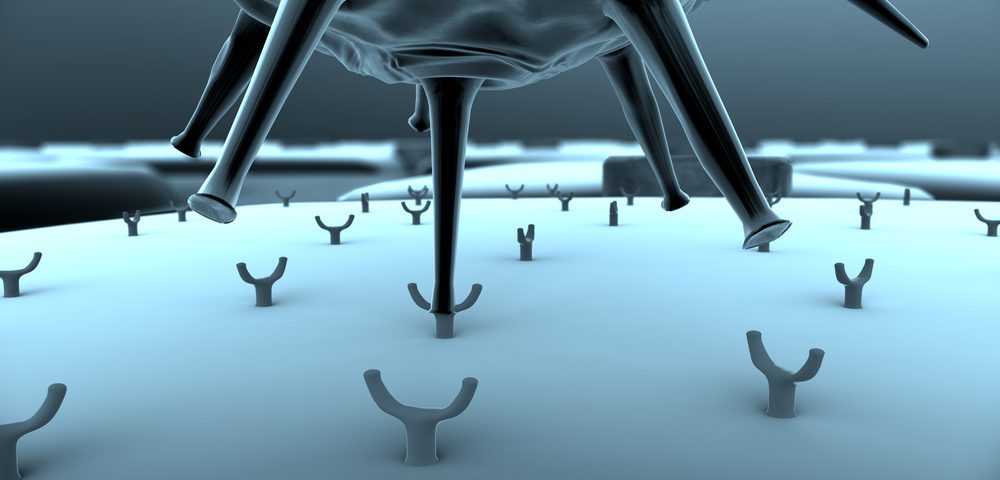
Researchers in Phase 1b trial evaluated the safety and efficacy of two drugs — ipilimumab, a cytotoxic T-lymphocyte antigen-4 inhibitor, and T-VEC, a systemically active oncolytic immunotherapy derived from the herpes simplex virus type-1 — in patients with untreated and unresectable advanced melanoma.
“Tumor immunotherapy has become an established treatment of metastatic melanoma and is being increasingly applied to other cancer types,” the authors wrote. “A hallmark of tumors likely to respond to immunotherapy is a lymphocyte-predominant tumor microenvironment. To date, immunotherapy designed to promote lymphocyte accumulation within established tumors, activate lymphocyte function and cytotoxicity, and prevent T-cell suppression has shown the most promise.”
A total of 19 patients, ages 29–84, were included in this study. Patients received T-VEC injections directly to their tumors on week one, week four, and every two weeks thereafter, plus four infusions of ipilimumab every three weeks, starting at week six. The primary endpoint was incidences of dose-limiting toxicities, and secondary endpoints were objective response rate (ORR) and safety. The median survival follow-up was 20 months, and patients treated with T-VEC had an median treatment duration of 13.3 weeks.
Results suggested no dose-limiting toxicities or new safety concerns, and both drugs were administrated at their full therapeutic dosage. All patients experienced side effects, five of them with grade 3. The most common side effects were chills (n=11), pyrexia (n=11), fatigue (n=9), diarrhea (n=8), pruritus (n=8), rash (n = 8), influenza-like illness, dehydration, and vomiting. The side effects were attributable to either ipilimumab or T-VEC.
The ORR was recorded as 50%, and four patients had a complete response, five had a partial response, and another four showed stable disease. All but one of these confirmed response patients had a response lasting six months or longer. Importantly, responses were observed in injected and uninjected lesions.
Median progression free survival (PFS) and overall survival (OS) have not been reached, but researchers estimated probabilities of 50% for PFS at both 12 and 18 months, and OS probabilities of 72% and 67% at 12 and 18 months, respectively.
“An ongoing, randomized phase 2 trial on the basis of this study comparing [T-VEC] plus ipilimumab with ipilimumab alone in patients with advanced melanoma is underway,” the authors added. “The combination of [T-VEC] with immune checkpoint inhibitors may represent potential new treatment options for patients with regionally or distantly metastatic melanoma with or without visceral disease that is injectable and cannot adequately be addressed by surgery.”