Immunotherapy has shown promise in eliminating the microtumors that sometimes remain after cancer surgery, but the treatment’s effects on other parts of the body have raised concern.
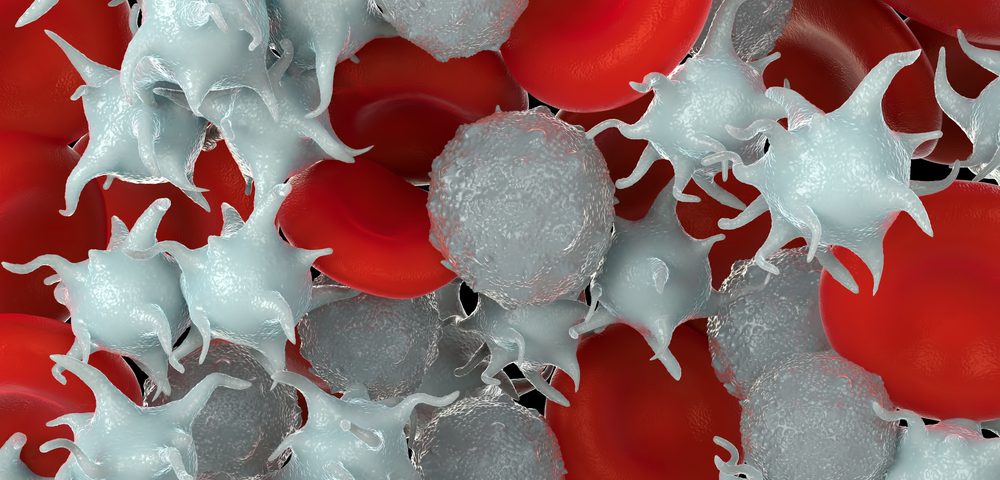
Platelets could be the answer, researchers have discovered. The tiny blood cells, which gravitate to the surgical site to start the healing process, can be loaded with immune-checkpoint inhibitors to activate the immune system at the site. That approach will leave other organs and tissue unharmed.
The study, “In situ activation of platelets with checkpoint inhibitors for post-surgical cancer immunotherapy,” was published in Nature Biomedical Engineering.
“There has been tremendous interest in developing new, effective strategies to prevent cancer recurrence after surgery,” Zhen Gu, PhD, the study’s senior author, said in a press release. “Among them, cancer immunotherapy has received considerable attention.” Gu holds joint faculty positions at the University of North Carolina School of Medicine, the UNC Eshelman School of Pharmacy, and North Carolina State University’s College of Engineering.
“But challenges remain in order for these [immunotherapy] inhibitor antibodies to be used effectively in patients,” said Chao Wang, PhD, a postdoctoral researcher on Gu’s team who was the lead study author. “Currently, the antibodies cannot target the tumor site effectively. The off-target antibodies and overdose usage of antibodies can cause side effects such as an autoimmune disorder, which can damage normal tissue cells.”
To overcome this problem, Gu’s team focused on developing a means to deliver immune-checkpoint inhibitors directly to residual tumors, rather than activating the immune system in a non-targeted way.
Platelets, the tiny blood cells involved in clotting, travel to injured sites to help in the recovery process. The researchers decided to assess whether platelets could be loaded with immune-checkpoint inhibitors to deliver therapies to a surgery site.
That approach would allow the immune system to become activated at the tumor site alone. Physicians could use the technique to eliminate microtumors and circulating tumor cells without patients experiencing the toxic effects associated with auto-immunity in other regions of the body.
“We wanted to utilize platelets’ intrinsic tendencies to accumulate at wounds and to interact with circulating tumor cells, for targeted delivery of immune checkpoint inhibitors” Gu said. “Interestingly, we found the antibody can be promoted to release from activated platelets in the surgical site, due to generation of small platelet-derived microparticles upon the platelet activation. Also, aggregated platelets can help attract and boost immune cells in the surgical site.”
The team partially removed used melanoma and triple-negative breast cancers in mouse models. They found that platelets carrying the PD-L1 inhibitor atezolizumab could release the treatment upon activation, significantly prolonging the mice’s overall survival after surgery.
Researchers believe this was a result of reduced risk of cancer regrowth and metastatic spread — or spreading to other parts of the body.
When the team simulated the metastatic process in the mice by injecting cancer cells in their blood, atezolizumab-loaded platelets fought the cells, preventing metastasis. Atezolizumab, marketed as Tecentriq, is currently approved to treat certain lung and bladder cancers, and holds promise as a therapy for several other cancers.
Platelets’ ability to fight circulating tumor cells means that loading them with immune checkpoint inhibitors may be a way to go after blood cancers as well as solid tumors.
“It’s going to be a broader technology to treat a variety of tumors,” Gu predicted. “That’s why we applied different cancer types — not just for solid tumors, but for cancers like leukemia. Leukemia is a liquid, circulating tumor, while breast tumors and melanoma are solid tumors, so this is going to be a very broad technology.”
“Dr. Gu’s work represents an exciting and elegant technological advance in targeted therapeutics for cancer,” said Melina Kibbe, MD, professor and chair of the department of surgery at UNC. “Engineering platelets to release PDL1 via microparticles overcomes several challenges currently facing cancer therapeutics. Specifically, Dr. Gu’s approach could avoid off-target systemic side effects by allowing for concentrated drug delivery at the site of interest. While much remains to be elucidated with this technology, there is great potential to have a dramatic impact on the care of patients with cancer.”