The radio-enhancer nanoparticle NBTXR3, which is being developed to treat seven types of cancer, can effectively engage patients’ immune systems to fight cancer, transforming “cold” tumors into “hot” tumors.
This is the first set of clinical data from Nanobiotix‘s immuno-oncology program, and suggests that NBTXR3 could potentially be used in combination with other immunotherapies to improve patient outcomes.
“Being able to transform cold tumors into hot tumors is one of the most challenging and promising topics in oncology,” Laurent Levy, CEO of Nanobiotix, said in a press release. “This preliminary clinical data indicates that NBTXR3 could play a key role in unlocking this potential. Given NBTXR3’s universal type mode of action and good safety profile, [it] could change the treatment landscape in numerous solid tumor cancers.”
While immunotherapies have shown promise in a variety of cancers, many patients fail to respond to these treatments. This is usually explained by a lack of immunogenicity — or the drug’s inability to generate an immune response.
NBTXR3 is a nano-sized compound designed to be administered directly into the tumor site, bound and captured by cancer cells, and enhance radiotherapy energy within the tumor tissue.
The compound is also known to generate intratumoral immunogenic cell death, a form of cell death that triggers the activation of the immune system. Researchers hypothesized that this could be key to engage a patient’s immune system into fighting the cancer cells.
To address that, Nanobiotix used the available samples collected from patients included in the company’s Phase 2/3 trial for soft tissue sarcoma (NCT02379845). The 26 participants were randomized to receive either NBTXR3 with radiotherapy or radiotherapy alone.
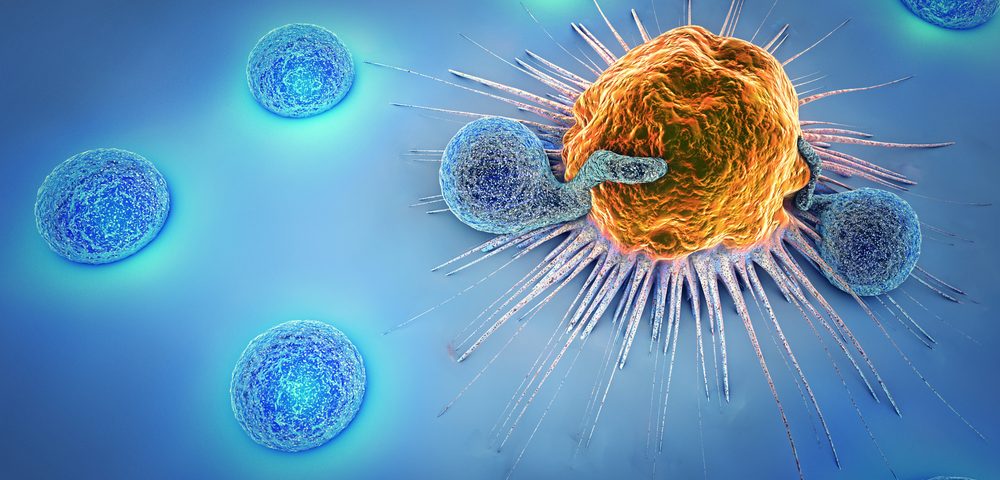
Looking at tumor samples collected before and after treatment, researchers found that patients who had received NBTXR3 had a significant increase in the number of T-cells inside the tumor compared to baseline. This difference, however, was not seen in patients receiving radiation therapy alone.
Similarly, patients in the NBTXR3 group had several signs of immune activation, including increased immune gene expression, increase in specific cytokines that activate the immune system, and in genes involved in adaptive immunity (the body’s first line of defense), and in T-cell signaling.
This data suggests that NBTXR3 is a potential immunotherapy that can trigger the immune system on its own. But the increase in immune-specific gene expression suggests that NBTXR3 could also be combined with other immunotherapy approaches, including immune checkpoint inhibitors.