Researchers have known that the checkpoint blockade therapies CTLA-4 and PD-1 inhibitors have been clinically successful in treating cancer patients. But they didn’t fully understand how these inhibitors function. A recent study has provided new insight into how CTLA-4 and PD-1 inhibitors work, and that could lead to new and better therapy strategies for patients.
The findings were published in an article titled, “Distinct Cellular Mechanisms Underlie Anti-CTLA-4 and Anti-PD-1 Checkpoint Blockade,” in the journal Cell.
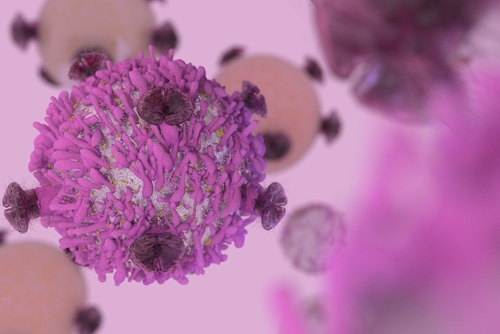
Anti-CTLA-4 and anti-PD-1 checkpoint-blockade therapies induce tumor rejection by activating and increasing the production of tumor-fighting T-cells. In this study, researchers from the University of Texas’ MD Anderson Cancer Center report that these immunotherapies act on distinct subsets of T-cells.
“The clinical successes of checkpoint blockade have gotten out ahead of our understanding of how these drugs work,” Jim Allison, PhD, chair of immunology at the MD Anderson Center and lead author of the paper, said in a press release. “In some ways, that’s a good problem to have, but we need greater understanding of the basic science behind these drugs to use them more effectively for patients.”
By better understanding the mechanism through which these treatments work, scientists could improve therapy strategies and physicians could determine the combination of drugs that works best for each patient. Allison’s research group conducted a series of experiments to discover the hidden mechanism behind the functioning of these therapies.
They used a technique called mass spectrometry, which allowed them to analyze the surface of cells and intracellular markers belonging to different subsets of T-cells, and to determine the composition of infiltrating immune cells in mouse tumor models treated with anti-CTLA-4 or anti-PD-1 therapies.
These experiments led to five main findings. First, administration of immune checkpoint blockade therapy resulted in the expansion of certain subsets of tumor-infiltrating T-cells.
Second, administering both anti-PD-1 and anti-CTLA-4 treatment expands the population of CD8 T-cells, which are potent killers of foreign pathogens. However, the PD-1-positive CD8 T-cells that emerge from this treatment exhibit an exhausted-like phenotype, which means that they likely are still functional, but inactive.
“These cells are boosted by anti-PD-1, but they keep their exhausted phenotype, which suggests they’ll shut down when the PD-1 antibody is withdrawn,” Allison said. This supports the need to maintain a PD-1 regimen for long periods of time.
Third, anti-CTLA-4 treatment, in addition to expanding the population CD8 T-cells, was also found to expand the ICOS-positive CD4 effector T-cells, which are a special subset that stimulates the immune system. Next, the researchers showed that the presence of these specific subsets of T-cells was associated with smaller tumors in mice, indicating that these T-cells play a role in tumor regression.
Finally, researchers showed that the subsets of T-cells that resulted from these specific therapies were consistent when treating different tumors in mouse models. Researchers analyzed samples of human melanoma tumors that were treated with anti-CTLA-4 and anti-PD-1 and showed that the same T-cell populations were expanded in these tumors as well.
This study highlights that specific tumor-infiltrating T-cell subpopulations are expanded when treated with the checkpoint therapies anti-PD-1 and anti-CTLA-4, and these are consistent across different tumors and species. Furthermore, these resulting subpopulations are associated with smaller tumors in mouse models.