Seattle Children’s Hospital has launched a new clinical trial, PLAT-05 (NCT03330691), and is currently recruiting participants to test a new CAR T-cell immunotherapy targeting two proteins expressed on cancer cells of certain patients with relapsed or refractory acute lymphoblastic leukemia (ALL).
Researchers hope the new therapy, targeting specifically the proteins CD19 and CD22, will slash the rate of relapse seen in these patients after undergoing CAR T-cell therapy by almost half.
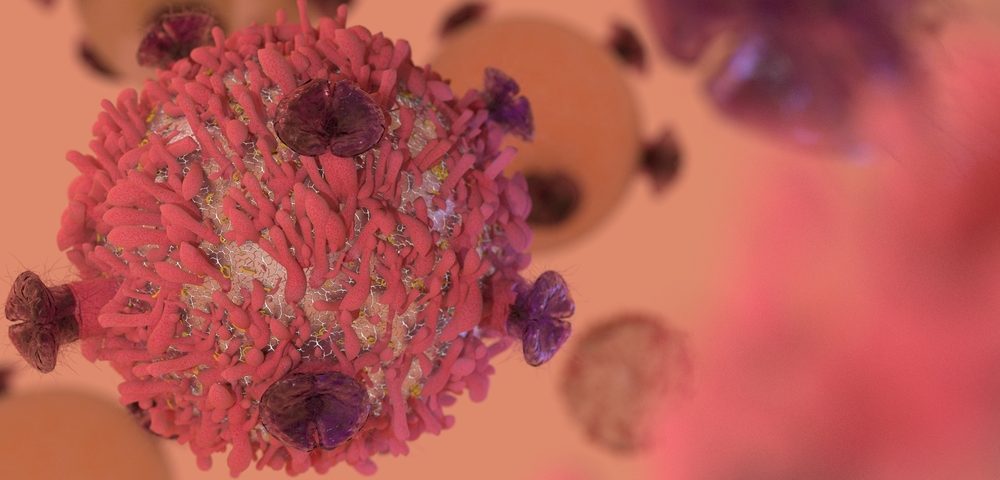
T-cells, the natural killers of our immune system, can be reprogrammed to express CARs on their cell surface by a gene editing process. These CARs direct T-cells to a specific antigen that is expressed on cancer cells, thereby leading the immune response to its intended target. When targeted to a specific cell type, T-cells proceed to destroy the cells.
In Phase 1 of the ongoing PLAT-02 (NCT02028455) clinical trial, also conducted at the Seattle Children’s Research Institute, patients with relapsed or refractory ALL using CAR T-cell immunotherapy targeting only the CD19 protein, achieved 93% remission. Unfortunately, approximately 50% of them relapsed after therapy.
Building from this data, researchers developed a two-pronged approach to target the cancer cells. During the PLAT-02 clinical trial, researchers determined that the relapses occurred either because the CAR T-cells were no longer persistent or the leukemia cells were able to circumvent the therapy.
This led them to conduct two new clinical trials – the PLAT-03 (NCT03186118), which aims to overcome the disappearance of T-cells – and the PLAT-05 (NCT03330691), which addresses the ability of cancer cells to circumvent the T-cells.
The idea behind the two pronged-approach is simple. Normally, the leukemia cells express a protein called CD19 on their cell surface. Therefore, the CAR T-cells are programmed to target CD19 and destroy the cancer cells.
Leukemia cells, however, can sometimes recur in a way that they are no longer expressing CD19 on their surface, and instead express another protein called CD22. Therefore, researchers were able to develop CAR T-cells that target both CD19 and CD22. This can lead to a reduction by almost 50% in relapse rates in these patients.
“This is an exciting time where we’re at the forefront of advancing the CAR T-cell immunotherapy field by pioneering strategies to improve long-term outcomes for children and young adults,” said Dr. Rebecca Gardner, lead researcher of the PLAT-05 trial in a press release.
“In launching a bilateral attack on the cancer cells, we hope this trial will help us develop a T-cell therapy that leads to long-term remission for many more of our patients,” said Gardner, who is also an oncologist at Seattle Children’s.
As CAR T-cell immunotherapy has been greatly successful, researchers are now looking to treat cancers that are traditionally more difficult to treat, such as solid tumors and sarcomas.
“We believe that T-cell immunotherapy holds tremendous potential to combat leukemia and several other types of pediatric cancer,” said Dr. Gardner. “Leukemia is just the tip of the iceberg, and we hope to develop a therapy that can be given to patients as a first line of defense, greatly reducing the side effects of cancer treatment.”