Melanomas with a high number of genetic mutations that lead to over-activation of the nuclear factor-κB (NF-κB) signaling cascade — a family of gene expression regulators — are about three times more likely to respond to treatment with checkpoint blockade immunotherapies, according to a study.
The findings were recently presented in the poster, “Investigating the role of NF-κB signaling and immune checkpoint blockade therapy in melanoma,” at the American Association for Cancer Research (AACR) Annual Meeting 2019 in Atlanta, Georgia.
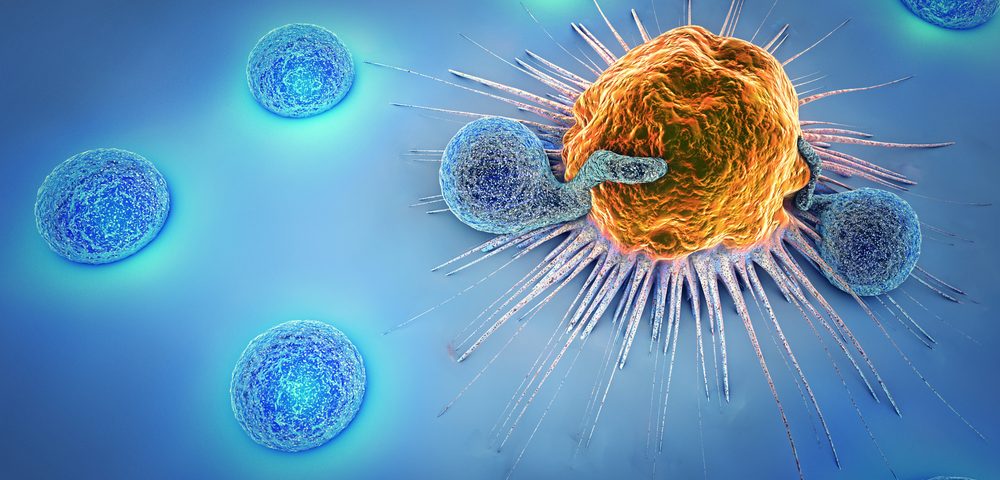
Checkpoint blockade immunotherapies are based on the principle of removing the “brakes” of our immune system and using its power to fight cancer faster and more effectively.
“Immune checkpoint blockade treatments, such as anti-PD1, improve survival in patients with metastatic melanoma (an aggressive form of melanoma that has spread to other tissues and organs). Despite durable response rates, 40-50% of patients show no benefit,” the researchers’ abstract states.
According to scientists, the reason half of melanoma patients fail to respond to immunotherapy may be because these tumors are “cold,” meaning they have low numbers of infiltrated immune cells. Conversely, patients with more aggressive forms of melanoma typically respond better because they have higher numbers of immune cells inside the tumor (“hot”), enabling immunotherapies to activate such cells.
One recurring problem in research and clinical practice is that distinguishing between a “hot” or “cold” melanoma can be extremely difficult. This is why physicians often start patients on immunotherapy as soon as they receive the diagnosis and hope for the best.
The problem with this approach is that inevitably the therapy will fail in some cases, leading to a waste of resources and time for all involved, in addition to some patients experiencing side effects.
One of the factors that may tip the balance toward the development of a “hot” tumor is the number of genetic mutations present in cancer cells. The idea is that if cancer cells accumulate a high number of genetic mutations, they become increasingly abnormal and chances are the immune system will be able to spot them faster and eliminate them.
However, a group of scientists from the University of Colorado Cancer Center believe they may have found an additional player in the process: the NF-κB signaling pathway.
“The NF-κB-pathway is important for immune response as a key transcription factor for several antigen presentation proteins and cytokine/chemokine (substances involved in immune and inflammatory response) production. This study explored NF-κB signaling in patients with favorable or unfavorable responses to anti-PD1 therapy,” the researchers said.
According to their findings, from the 52 patients with metastatic melanoma participating in the study, 21 responded to anti-PD-1 immunotherapy, and 31 failed to show any improvement.
As expected, whole-exome sequencing (WES) analysis — a method that examines DNA sequences of all genes encoding for proteins — revealed that patients who responded to anti-PD-1 immunotherapy had a higher number of genetic mutations in melanoma cells, compared with those who failed to respond to therapy.
But WES also showed that 67% of the patients who responded favorably to anti-PD-1 immunotherapy had significant alterations in the NF-κB signaling cascade, compared to 19% of those who failed to respond.
“NF-kB is a complex pathway — sometimes it’s bad (because it may aggravate cancer) and sometimes it’s good (because it makes it easier for immunotherapies to target cancer). The cell context may be different than the treatment context. What we show is that cancers with alterations that over-activate the NF-kB may better benefit from immunotherapy,” Carol Amato, MS, investigator at CU Cancer Center and senior professional research assistant, said in a press release.
Further analysis showed that patients whose melanoma responded to therapy had a genetic mutation (G34E) in NFKBIE — a negative regulator of NF-κB — that led to an over-activation of NF-kB, which in turn increased the expression of another gene called CD83.
“And it’s CD83 that we think is enhancing responsiveness of the tumor to immunotherapy,” Amato said.
Interestingly, when researchers artificially increased the number of NFKBIE G34E mutations, they saw that NF-κB signaling activity increased, regardless of the number of other genetic mutations also present in the tumor.
“Even beyond tumor mutation burden, these specific changes could help doctors predict which melanoma patients will respond and which patients will not respond to anti-PD1 immunotherapies,” Amato said.