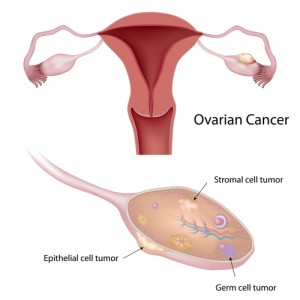
 Epithelial ovarian cancer (EOC) is considered the most lethal gynecologic malignancy in women, with a relapse rate of approximately 85% and a 5-year overall survival of 20–30%. The poor clinical outcome in this kind of cancer has led the scientific community to search for targeted treatment strategies, such as immunotherapy.
Epithelial ovarian cancer (EOC) is considered the most lethal gynecologic malignancy in women, with a relapse rate of approximately 85% and a 5-year overall survival of 20–30%. The poor clinical outcome in this kind of cancer has led the scientific community to search for targeted treatment strategies, such as immunotherapy.
In a recent study entitled “Expression and Immune Responses to MAGE Antigens Predict Survival in Epithelial Ovarian Cancer” and published in the journal PLOS ONE, researchers from the Roswell Park Cancer Institute (RPCI) observed that the melanoma-associated (MAGE) cancer-testis antigens (CTAs) expression patterns correlate with established clinical outcomes in epithelial ovarian cancer.
Cancer testis antigens (CTA) are a subclass of tumor-associated antigens (TAA), which are encoded by approximately 140 genes. Even though their biological function is not well characterized, they are known to be expressed in sites such as the testes, placenta and fetal ovary, but not in other normal tissues. Abnormal expression of these genes in malignant tumors can lead to tumor progression and increased immunogenicity, a characteristic that has lad to the development of cancer vaccines aimed specifically at targeting these antigens, especially the MAGE family of proteins.
In this study, the researchers examined 5 MAGE molecules’ expression patterns by utilizing genetic and immunohistochemical screens 400 ovarian cancer patients’ tissue samples.
Antibody recognition patterns were then analyzed, revealing that “abnormal expression of MAGE-A1 was present in 15% of epithelial ovarian cancers, expression of MAGE-A3 was present in 36%, expression of MAGE-A4 was present in 47%, expression of MAGE-A10 was present in 52%, and expression of MAGE-C1/CT7 was present in 16%. Furthermore, co-expression of MAGE-A1 and MAGE-A10 correlated with poor overall progression-free survival. Conversely, MAGE-C1/CT7 was shown to improve progression-free survival.”
The researchers concluded that this type of TAAs can become future prognostic factors for ovarian cancer, while MAGE-A4 in particular, could become a priority target for ovarian cancer immunotherapy.
The next step is to translate this type of research into the clinic, allowing the development of new and improved treatment options for patients suffering from ovarian cancer, as well as patients with other MAGE-positive cancers, such as melanoma, breast cancer and lung cancer.


