 During the European Society for Medical Oncology (ESMO) congress 2014, Madrid, different studies highlighted the importance of tumor infiltrating lymphocytes (TILs) in cancer prognostic and treatment.
During the European Society for Medical Oncology (ESMO) congress 2014, Madrid, different studies highlighted the importance of tumor infiltrating lymphocytes (TILs) in cancer prognostic and treatment.
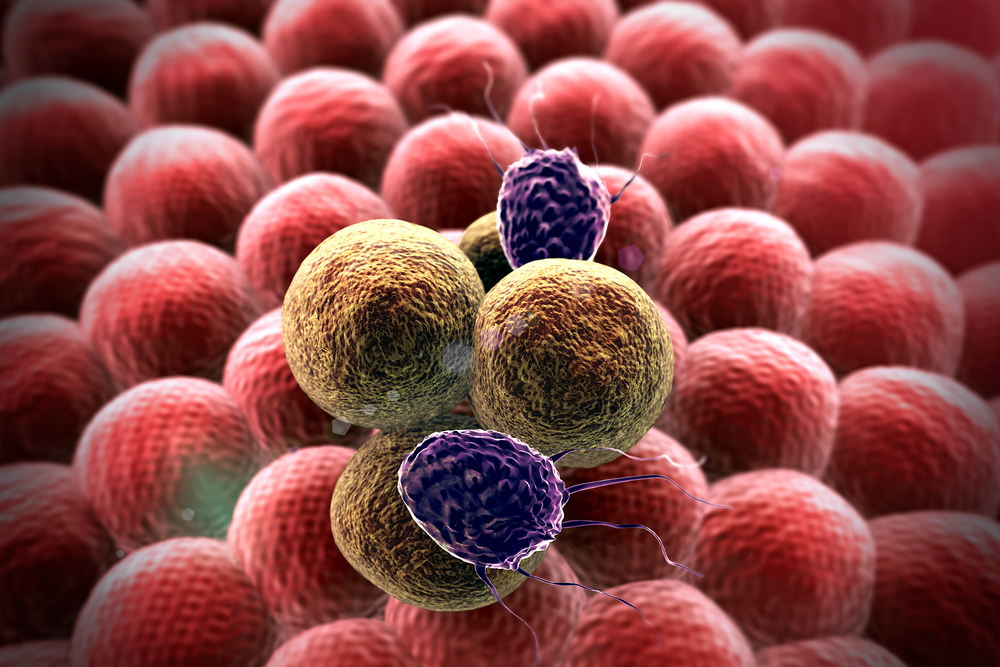
The tumor microenvironment is composed of endothelial, structural and several immune cells, which can be manipulated by the tumor itself in order to account for its own metabolic and immunological necessities.
TILs are recruited into the tumor microenvironment in an attempt to control tumor growth and eventually destroy tumor cells.
Studies have demonstrated that the amount of TILs during cancer diagnosis can be associated with prognosis. Furthermore, these cells can be manipulated into a treatment for that patient’s cancer.
In one of the ESMO sessions, Dr. Rikke Andersen from Herlev Hospital, Denmark, presented the results from a phase II clinical trial assessing low-dose IL-2 in patients receiving TILs for metastatic melanoma. The results demonstrated an overall low toxicity, with 2 complete and 7 partial responses, 2 of which persisted beyond 2 years, resulting in an overall response rate of 45%.
Moreover, adoptive cell therapy with TILs induced some immunological memory, with these immune cells demonstrating in-vitro cytotoxicity against melanoma cells.
Data from several studies in different types of cancers has demonstrated that tumor infiltration by CD8 T cells, Th1 and Th17 CD4 T cells, natural killer (NK) cells, dendritic cells (DC) and M1 macrophages, is a positive predictor of diagnosis. On the contrary, tumor infiltration of CD4 regulatory T cells (Tregs), Th2 CD4 T cells, myeloid-derived suppressor cells (MDSC), M2 macrophages and neutrophils, is commonly associated with a poor prognosis.
Tumor-associated antigens expressed by cancer cells are normal proteins expressed in significantly higher amounts than in normal cells, and therefore, are tolerated by the immune system.
Due to immune selection of genetically unstable tumour cells, resistant variants emerge which are no longer recognized by adaptive immunity, for example due to antigen loss, becoming insensitive to immune surveillance and inducing tolerance within the tumour microenvironment. These resistant tumor cells can then re-emerge after therapy and progress towards a metastatic stage of the disease.
Results from a clinical trial in triple-negative breast cancer (TNBC) showed a positive association between the number of TILs present in diagnosis and prognosis in TNBC but not in luminal or HER2-positive subtypes. Furthermore, an interaction between higher levels of TILs and trastuzumab use was also observed, with an 18% reduction in the relative risk of distant recurrence for each 10% increase in lymphocyte infiltrates.
Over the last few years, there has been a significant amount of data concerning genes and proteins associated with the immune system, as well as multiple clinical trials addressing the use of checkpoint inhibitors in the treatment of multiple types of tumors. Even though a number of issues remain to be addressed, results so far have been encouraging, with immunotherapy proving to be a strong and essential ally in cancer research.