In a recent study entitled “Immunosuppressive plasma cells impede T-cell-dependent immunogenic chemotherapy,” researchers discovered that immunosuppressive B cells allow advanced prostate tumors to resist chemotherapy. The team showed that once these B cells are removed, prostate tumors become sensitized to therapy and are almost completely destroyed. The study was published in the April 29 issue of the journal Nature.
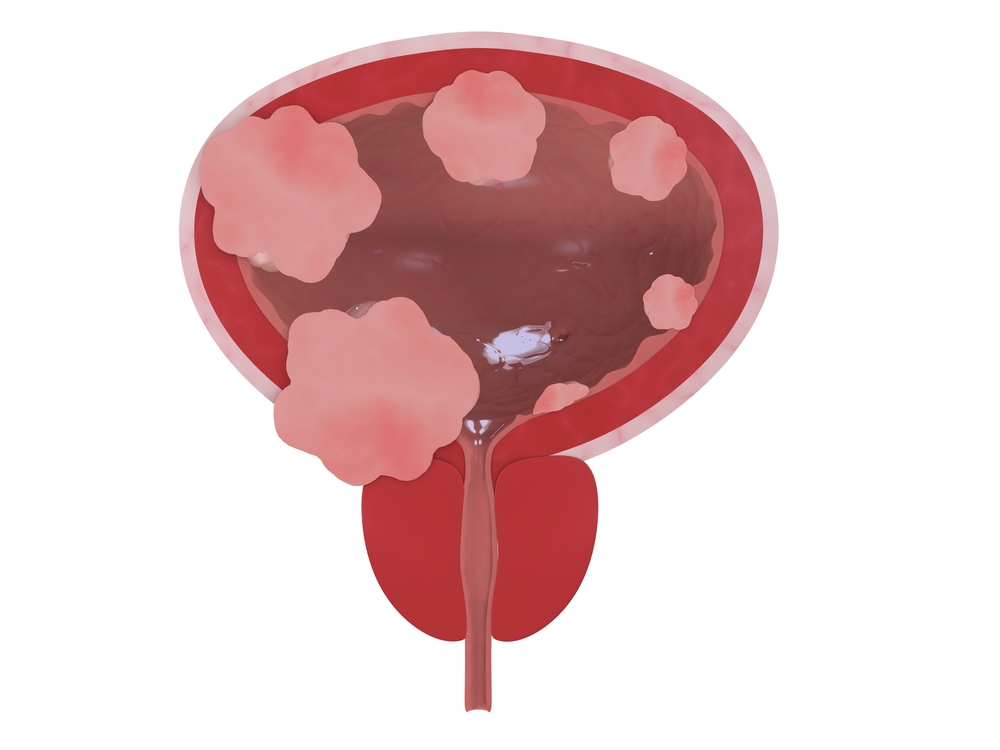
Advanced or metastatic prostate cancer is particularly difficult to treat, usually because the tumors have acquired, not only resistance to chemotherapy, but also to checkpoint inhibitors, an immunotherapy-based strategy that unlocks the patients’ immune system to fight the tumor more efficiently. Large and advanced prostate tumors develop immune resistance by recruiting and hijacking certain immune-checkpoint players, such as immunosuppressive B cells — these cells are responsible for inhibiting or preventing activation of the immune system, halting therapeutics that allows tumors to keep growing.
In the study, researchers at the University of California San Diego (UCSD) studied how B cells influenced the acquisition of chemotherapy resistance in advanced prostate cancer, and they focused on oxaliplatin, a chemotherapy drug that activates immune cells directed to killing tumor cells, and an effective agent in aggressive prostate cancer. The team used three different mouse models of advanced prostate cancer, and discovered that by blocking immunosuppressive B cell functions, or by removing these cells completely before low-dose oxaliplatin treatment, prostate tumors were effectively targeted by mouse immune system and destroyed. Only upon depletion of B cells (either genetically or with drugs) did mice become sensitized to oxaliplatin. The same phenotype was observed when the researchers coupled low-dose oxaliplatin with a checkpoint inhibitor.
As a result, the teams’ findings unveil a critical role for immunosuppressive B cells in maintaining tumors resistance to immunogenic chemotherapy.
Shabnam Shalapour, PhD, study first author noted, “The presence of such B cells in human prostate cancer calls for clinical testing of this novel therapeutic approach.”
Michael Karin, PhD, Distinguished Professor of Pharmacology and Pathology at UC San Diego and study lead author added, “In addition to prostate cancer, similar immunosuppressive B cells can be detected in other human cancers. This indicates that B cell-mediated immunosuppression might be the reason several other cancers are also unresponsive to checkpoint inhibitors, raising the hope that chemoimmunotherapy will have broader applications for many cancer types.”