A new study entitled “M1 Macrophages Demonstrate a Superior Phagocytic Response Against Glioblastoma Multiforme Following Anti-CD47 Treatment” was recently presented at the 2015 edition of the American Association of Neurological Surgeons (AANS) Annual Scientific Meeting, held from May 2-6 in Washington, D.C.
The study, presented by Michael Zhang, the recipient of the Medical Student Summer Research Fellowship Award, focused on the role of a type of macrophages in the pathogenesis of Glioblastoma Multiforme, the most aggressive form of brain tumor affecting adults.
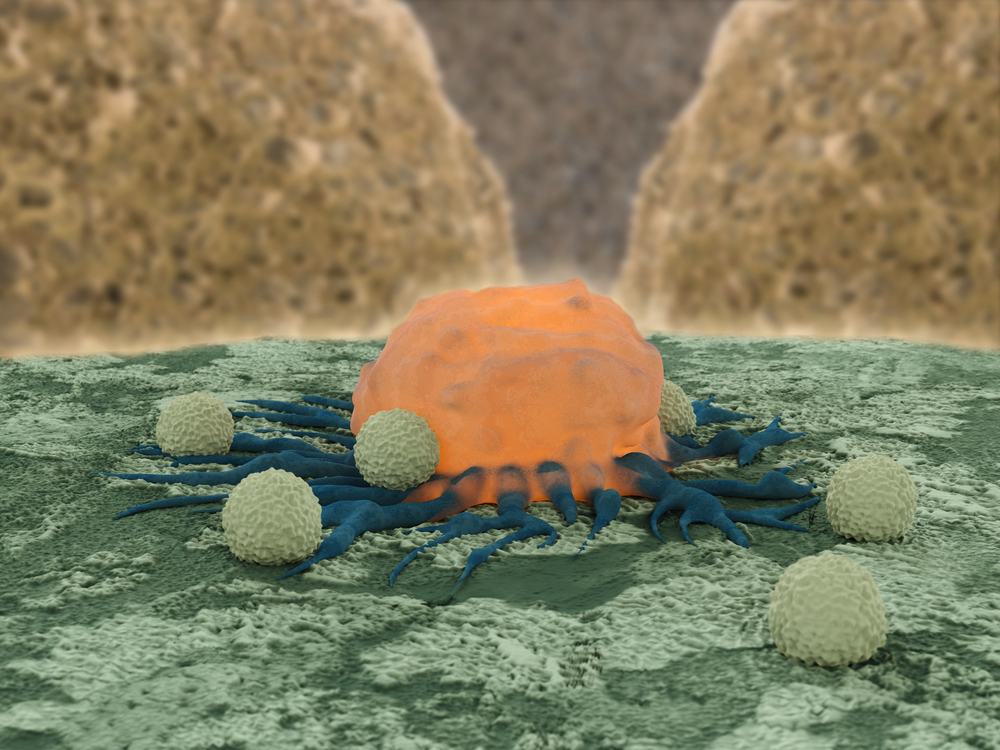
CD47, an integrin-associated protein, is over-expressed in several tumors, including glioblastoma multiforme. Its expression at the surface of cells is used as a mechanism to protect itself from phagocytosis (a process of ingestion) by macrophages, a type of white blood cell that engulfs and digests damaged and abnormal cells, as well as foreign substances and pathogens. Specifically, CD47 when expressed at the cell surface binds to the signal regulatory protein-a (SIRP-a), a protein expressed by macrophages, triggering a signaling cascade that culminates with the inhibition of the phagocytic process.
Past studies showed in mouse models of Glioblastoma Multiforme that when these mice were treated with anti-CD47 antibodies, the mice survived for longer periods of time. However, usually a tumor’s microenvironment exhibits a heterogeneous macrophage population, including both M1 and M2 macrophages that function in a variety of ways: while M1 macrophages are pro-inflammatory, enhancing immune responses against tumor cells, M2 macrophages are pro-tumoral, since they express a wide array of anti-inflammatory molecules, providing an immunosuppressive microenvironment and fostering tumor growth.
In this study, researchers performed co-cultures of different cell types, specifically, M1 and M2 mouse and human macrophages with tumor cells either treated with or without anti-CD47 antibodies. The cells were then treated with specific identifying markers to distinguish each cell population and were analyzed using flow cytometry. The team also performed in vivo studies using mice that were previously implanted with glioblastoma multiforme xenograft, and then quantified the frequency of M1 macrophages in the region surrounding the tumor in two conditions — mice randomly assigned to receive therapy with or without the anti-CD47 antibody.
The team observed that in vitro, treating co-cultures with anti-CD47 antibodies significantly increased the rate of phagocytosis by M1 macrophages in relation to the M2 population, specifically from 0.45 to 1.47. Of note, the anti-CD47 therapy resulted in an increase in phagocytosis for both macrophage subtypes. The in vivo experiments showed that mice randomly assigned to receive anti-CD47 therapy exhibited a peritumoral macrophage population significantly enriched in M1-like macrophages when compared to the control therapy (72.2% against 33.7%, respectively).
As a result of these findings, anti-CD47 therapy may become a promising therapy for enhancing survival of patients with Glioblastoma Multiforme.