In a new study entitled “Genetic absence of PD-1 promotes accumulation of terminally differentiated exhausted CD8+ T cells”, published in the Journal of Experimental Medicine, researchers show that T cells, key cells of the immune system, develop “T cell exhaustion” rendering them less capable of fighting cancer or infections.
The team showed that contrary to some suggestions, the protein PD-1 is not required for the induction of T cell exhaustion and may actually protect T cells from “burning out”. The inhibitory receptor Programmed Death1 (PD1) is an essential regulator of T cell activity and, in short-term infections, PD-1 expression helps to control T cells’ over-proliferation, preventing an auto-immune attack. However, while in short-term infections blocking PD-1 inhibits cells’ proliferation, in other more permanent disease settings, like in cancer or chronic infections, PD-1 was shown to have detrimental effects.
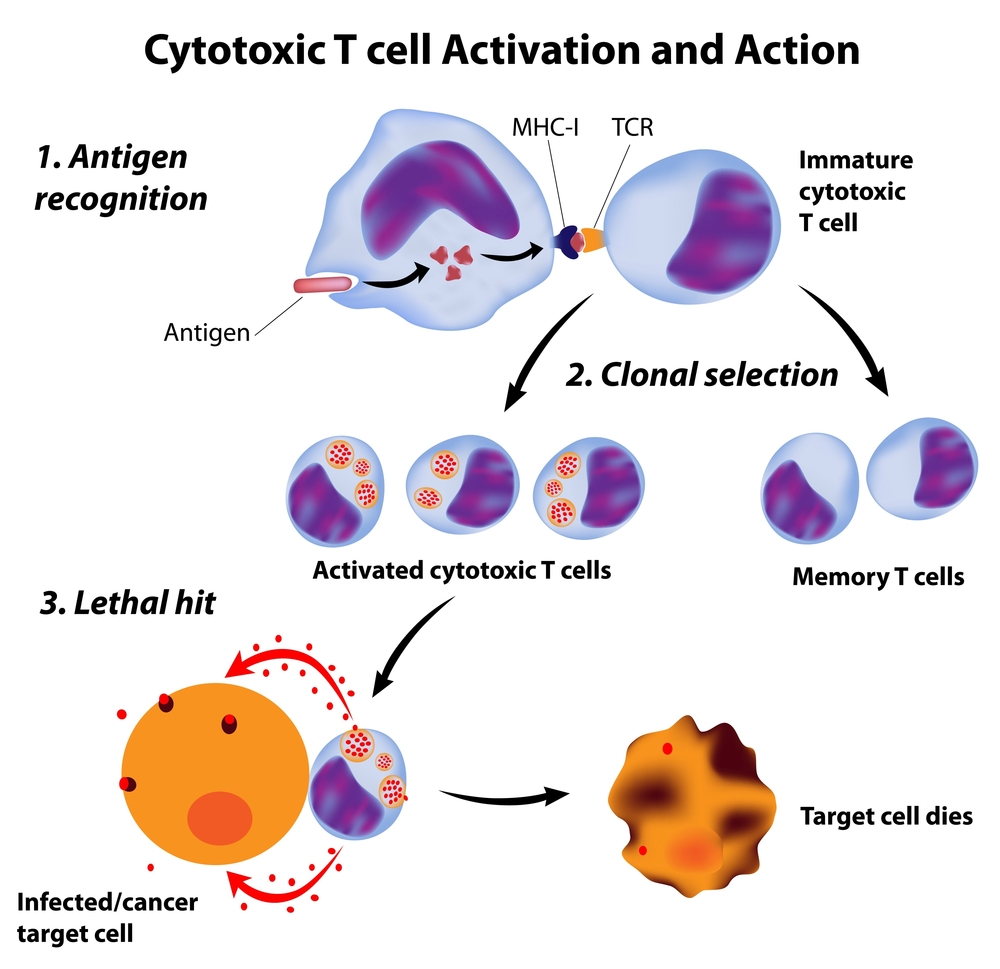
However, whether PD-1 actually promoted T cell exhaustion or not was still an open question. In this study, a team of researchers led by E. John Wherry, PhD, a professor of Microbiology and Director of the Institute for Immunology, in the Perelman School of Medicine, University of Pennsylvania tackled this issue. The team infected PD-1 knockout mice (mice that were genetically engineered to not express PD-1) with a lymphocytic choriomeningitis virus. The team wanted to determine if PD-1 was the cause for T cell exhaustion. They observed that genetic deletion of PD-1 resulted in higher T cell exhaustion from infection onset. Specifically, the team discovered that after an initial robust T cell response, these cells are incapable of keeping a high activation status, therefore becoming dysfunctional.
The team showed that T cell exhaustion can actually occur in the absence of PD-1. MoreoverPD-1 may help preserve a “T cell reserve” to fight infections or tumor cells in later stages.
As Dr. Wherry noted, “While transient disruption of this pathway may have therapeutic benefit because it temporarily ‘revs up’ the immune response, permanent loss of PD-1 signals seems to result in a ‘flame out’ where T cells can’t sustain higher level activation and become more dysfunctional.”