Immunotherapy using genetically modified immune T-cells (CAR-T) to specifically target the glioma-associated marker IL13Rα2 — a gene expression indicative of an aggressive brain tumor — was reported to be a successful treatment for recurrent multifocal glioblastoma in a case study recently published in the New England Journal of Medicine.
CAR-T immunotherapy has demonstrated efficacy in treating hematological malignancies, but its effectiveness and clinical applicability for solid cancers is yet to be established. Researchers from the City of Hope cancer center have started a Phase 1 clinical trial (NCT02208362) to evaluate the safety and therapeutic potential of this approach for the treatment of aggressive brain tumors. (The study, at the Duarte, California, center, is recruiting patients.)
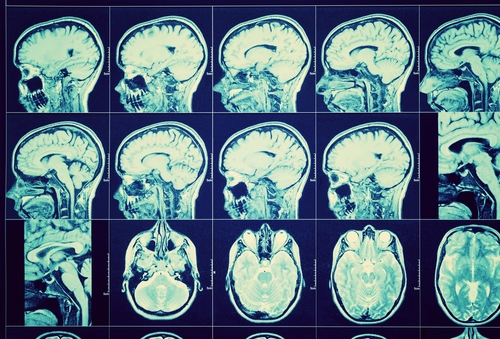
In the article “Regression of Glioblastoma after Chimeric Antigen Receptor T-Cell Therapy,” the authors presented findings from the use of this new therapeutic regimen in one patient with recurrent multifocal glioblastoma, affecting both the brain and the spinal cord, who previously did not respond to standard-of-care therapy that included resection, radiation, and chemotherapy with Temodar.
This CAR-T therapy regimen required direct delivery of the CAR T-cells to brain tumors for 220 days via a catheter device. No severe toxic effects, of grade 3 or higher, were reported in this case study. Mild toxicity effects such as headaches, generalized fatigue, muscle pain, and olfactory auras were reported within 72 hours after treatment.
“By injecting the reengineered CAR-T cells directly into the tumor site and the ventricles, where the spinal fluid is made, the treatment could be delivered throughout the patient’s brain and also to the spinal cord where this particular patient had a large metastatic tumor,” said the study’s co-senior author, Behnam Badie, MD, chief of neurosurgery at City of Hope.
Overall, a regression of both brain and spinal tumors was observed with significant improvements in the patient’s quality of life, allowing a return to normal life activities. The researchers also observed that the patient’s general immune response improved upon treatment, with increased levels of immune cells in the cerebrospinal fluid. This clinical response was maintained for 7.5 months after initiation of CAR-T cell therapy.
These results give promising support to future use of intracranial CAR-T cell therapy as means of preserving patients’ neurological functions and minimizing the toxic side effects of other treatments.
“City of Hope has accepted the challenge to try to make a therapy that can be used for patients with many different types of cancers,” said Stephen J. Forman, MD, director of City of Hope’s T-cell Immunotherapy Research Laboratory and the study’s co-senior author. “Our CAR-T program here is focused not only on leukemia, lymphoma and myeloma, but also on solid tumors including breast cancer, liver cancer and brain cancer, as a way to try to make effective immunotherapy options for difficult-to-treat cancers.”
Promising results presented in the study have prompted an expansion of the Phase 1 trial, now evaluating the efficacy of intra-ventricular administration in a larger cohort of patients.