Immune checkpoint inhibitors targeting the PD-L1 molecule appear to activate immune cells called natural killer (NK) cells, a new study says. This finding may explain why some tumors are responsive to these checkpoint inhibitors even when the PD-L1 checkpoint protein isn’t expressed.
The new study, “The mechanism of anti-PD-L1 antibody efficacy against PD-L1 negative tumors identifies NK cells expressing PD-L1 as a cytolytic effector,” was published in the journal Cancer Discovery.
Checkpoint inhibitors are a class of anticancer therapeutics that has gained a lot of attention in recent years. As the name suggests, these inhibitors work by blocking checkpoint molecules: basically, some healthy cells produce molecules that work as a “don’t attack” signal to the immune system, most notably T cells. This is meant to prevent immune cells from killing healthy cells, but cancer cells often co-opt this system so they can avoid immune system-mediated destruction.
One of the most well-understood checkpoint systems is the PD-1/PD-L1 system: PD-1 is expressed by immune cells and recognizes PD-L1, which many cancer cells express.
Interestingly, checkpoint inhibitors that block PD-L1 have shown some positive results in tumors that don’t express PD-L1. This is puzzling because, in theory, there’s nothing for the inhibitor to inhibit. But the new study may have uncovered a hitherto unknown mechanism by which PD-L1 inhibitors can affect the immune system to facilitate cancer cell killing, independent of PD-L1 on tumors: by activating NK cells.
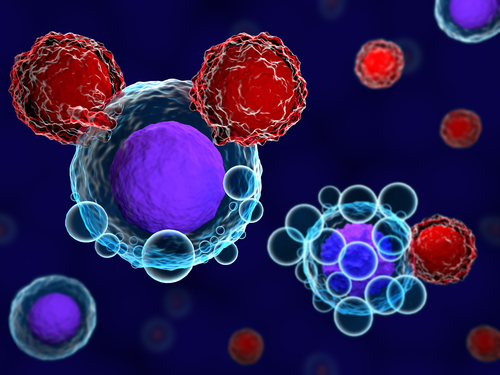
“Natural killer cells are the body’s first line of defense against cancer and viral infections,” Michael Caligiuri, MD, president of City of Hope National Medical Center and a co-author of the study, said in a press release. “When NK cells detect tumor or viral cells in the body, they have the potential to kill them immediately. But in those with cancer, tumors have developed mechanisms to circumvent NK cells.”
When the researchers exposed human NK cells to cancer cells in a dish, the NK cells started expressing PD-L1, regardless of whether or not the cancer cells did. Furthermore, the NK cells that expressed PD-L1 had more markers of activation than those that didn’t, suggesting that PD-L1 is expressed by some NK cells when they become activated.
The researchers also looked at NK cells taken from 79 individuals with acute myeloid leukemia (AML). PD-L1-positive NK cells were found in 77% of these, but none were found in 48 healthy volunteers.
Additionally, among the people with AML who went into complete remission following standard chemotherapy, the number of PD-L1-positive NK cells was significantly higher than at diagnosis. But there was no significant change in the frequency of PD-L1-positive NK cells among people with AML who did not go into remission.
These data further suggest that PD-L1 expression is a marker of activated, cancer-killing NK cells —might this be harnessed therapeutically?
When the researchers treated PD-L1-positive NK cells with Genentech‘s PD-L1 inhibitor Tecentriq (atezolizumab), the cells showed further signs of activation, presumably because Tecentriq was binding to, and therefore activating, PD-L1 on NK cells.
Of note, the “inhibitor” part of “PD-L1 inhibitor” refers to blocking cross-talk between cells; once bound to PD-L1, the molecule may actually promote signaling within PD-L1-positive cells.
The researchers then tested the efficacy of this strategy in mice. They found that Tecentriq treatment had an anti-tumor effect in mice with PD-L1-negative tumors. Importantly, though, this effect was not seen in mice that couldn’t make their own PD-L1 or that didn’t have NK cells.
These data suggest that it is the NK cell-activating activity of PD-L1 inhibitors that makes some PD-L1-negative tumors responsive to this checkpoint therapy.
“We have provided a scientific explanation as to how checkpoint inhibitor therapy can work when there’s no checkpoint expressed on a patient’s cancer cells,” said City of Hope professor and study co-author Jianhua Yu, PhD. “Using checkpoint inhibitors for NK cells with PD-L1 expression can lead to stronger anti-cancer activity, providing us with another powerful therapy against even more cancers.”