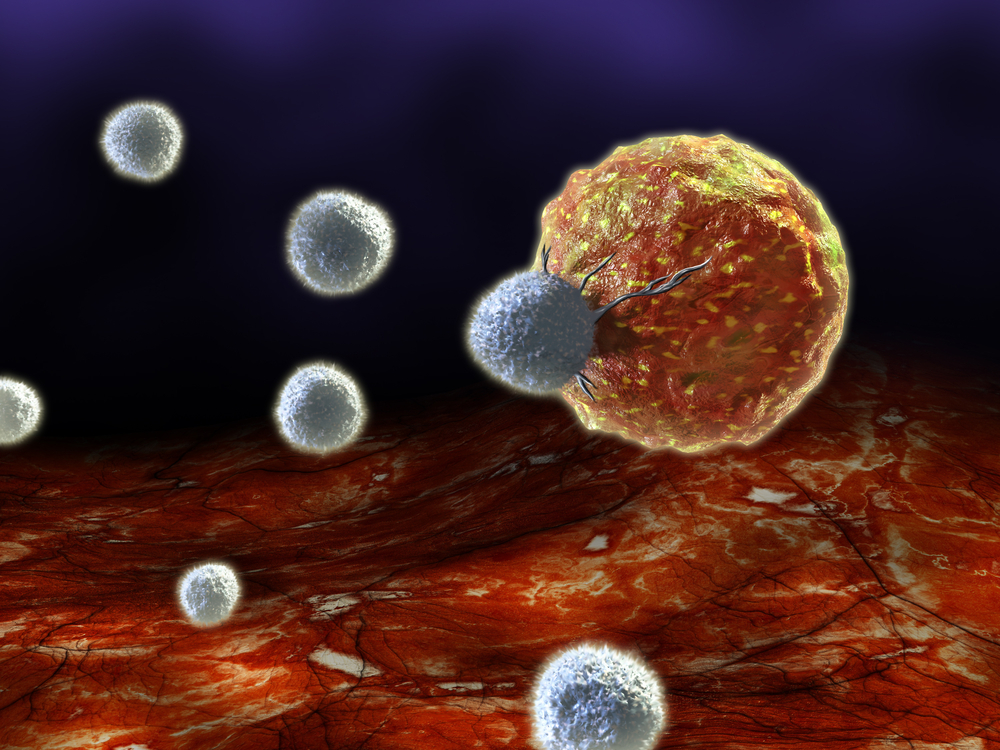
 In a recent study, titled “Cancer Immunotherapy Employing an Innovative Strategy to Enhance CD4+ T Cell Help in the Tumor Microenvironment”, published in PlosOne, a research team from Johns Hopkins Medical Institutions have investigated whether intratumoral injection of PADRE peptide (the pan HLA-DR binding epitope) along with adjuvant CpG following cisplatin chemotherapy could result in strong antitumor effects and antigen-specific cell-mediated immune responses.
In a recent study, titled “Cancer Immunotherapy Employing an Innovative Strategy to Enhance CD4+ T Cell Help in the Tumor Microenvironment”, published in PlosOne, a research team from Johns Hopkins Medical Institutions have investigated whether intratumoral injection of PADRE peptide (the pan HLA-DR binding epitope) along with adjuvant CpG following cisplatin chemotherapy could result in strong antitumor effects and antigen-specific cell-mediated immune responses.
The PADRE peptide has been shown to generate antigen-specific CD4+ T cells that can bind various MHC class II molecules (present in the majority of tumor cells) with high affinity. Furthermore, this peptide has also been used in combination with vaccines to augment their potency, enhancing CD4+ T cell responses.
As such, the authors hypothesized that intratumoral administration of PADRE could allow PADRE-specific CD4+ T helper cells to increase cross-presentation and further enhance a tumor antigen-specific CD8+ T cell response.
To test their hypothesis, the team used mice that had been injected with tumor cells (HPV16 E7-expressing TC-1 tumors) and preceded to treat them using a combination of cisplatin followed by intratumoral injection with CpG (a toll-like receptor 9 agonist shown to stimulate CD8+ T cell cross-priming through type I interferon production) and PADRE peptide.
They observed that the most powerful treatment was upon combination of all different agents, which was capable of controlling tumors at a distant site, through immune cross-presentation of the tumor antigen.
Additionally, they found that cisplatin, CpG and PADRE treatment was capable of enhancing the production of PADRE-specific CD4+ T cells along with E7-specific CD8+ T cells.
According to the authors, the therapeutic approach described in this study, “is a novel application of a combination of immunotherapies that induces potent antitumor immune responses without requiring knowledge of immunodominant tumor antigens, making the approach potentially widely applicable. This strategy may serve as a platform technology for the treatment of a variety of cancers, potentially including metastatic cancer. Additional studies will be needed to further enhance the stimulated immune responses and to extend the approach to inaccessible tumors”.